Medical equipment budgeting
 Key to the success of a health care construction project is a vetted and approved medical equipment budget. This lays the foundation for the application of practices that may not only save the facility money on medical equipment, but on the entire project cost.
Key to the success of a health care construction project is a vetted and approved medical equipment budget. This lays the foundation for the application of practices that may not only save the facility money on medical equipment, but on the entire project cost.
This requires careful consideration of a number of important variables such as the sophistication of the equipment being specified, the accuracy of cost estimates, the needs and desires of the various stakeholders and the frequency of change orders, to name a few.
Successful professionals will take a formal approach to ensuring that these and other concerns are properly addressed.
Budget development
Historically, medical equipment budgets for health care construction projects were determined as a percentage of projected construction cost. The industry now recognizes that two hospitals with the same square footage can offer completely different services, resulting in significant differences in the cost for owner-furnished medical equipment.
A more accurate method than basing a budget on square footage is basing it on a space program. But, even then, the budget may vary significantly, depending on a variety of factors.
A fundamental concept in developing the medical equipment budget is the budget-setter’s definition of medical equipment — not just categories of devices but whether factors such as relocation costs, equipment upgrades, leases, transition rentals, information technology (IT) integrations and ancillary expenses (i.e., electronic health record interoperability) will be part of the medical equipment budget.
Additionally, the project delivery method (i.e., design-build, integrated project delivery or design-bid-build) may impact the procurement process and the final cost of medical equipment. On a design-build project, for instance, medical equipment that typically is considered owner-furnished may be furnished by the contractor.
The construction schedule also can impact the cost of medical equipment. For example, in renovation or expansion projects, phasing can impact the warehousing requirements, equipment discounting and the practicality of relocating existing equipment versus purchasing new equipment.
After all these issues are considered, the health care organization will determine whether the budget should include additional costs such as tax, freight, inflation, group purchasing organization (GPO) discounting, insurance for stored equipment, warehousing costs, installation, transition planning and various contingencies.
Cost estimate
The cost estimate encompasses many of the same or similar parameters as the budget as well as clinical input, design-driven decisions, supply chain considerations and other factors. The best process to assemble this information is to gain input through a series of meetings.
Pre-design visioning sessions. Before design meetings begin, the organization should document the technology vision for the facility. It is important that all participants in the design process (e.g., administrative personnel, clinical directors and physicians) understand and support the organization’s vision. A large, urban teaching or research facility might include cutting-edge medical equipment or specialized technology such as positron emission tomography (PET), teaching surgical suites, interoperative surgical suites or research laboratories. In other circumstances, a critical access hospital’s market may not require PET, but the organization may want to consider technologies such as telemedicine.
If an organization is considering implementing a Lean program, medical equipment planning for the new facility can support that effort. Likewise, if an organization has not already established medical equipment standards, a new project is an ideal opportunity to start. These programs may allow the health care organization to realize better pricing. Additionally, maintenance and staff training may be reduced.
The project team should begin by identifying the budget and cost-estimate decision-makers and ask them to establish who is carrying what costs in their budgets. For instance, picture archiving and communication system display monitors may be carried in the IT cost estimate or in the medical equipment estimate. The team also should meet with supply chain and purchasing early in the design process to understand GPO contracts, standards, leased and no-charge items and discounting expectations.
The team also should discuss who will be responsible for installing no-charge items like glove boxes and sharps containers. Vendors can assume this role, but contractors might be the better choice because they are involved in mock-ups and understand the planning of the room and placement. Vendors inadvertently may place items in the wrong position and cause reworking of walls.
Capital purchases already approved and capital budgets in the years leading up to project completion should be considered during project design to help alleviate budget shortfalls. Similarly, it is important to determine whether the project is relocating equipment from another facility. The decision-makers should establish which categories of equipment should be considered for relocation.
Clinical user meetings. Medical technology user involvement is essential to developing a reliable cost estimate. The right clinicians and staff members should be brought to the design and planning meetings. For example, a nurse might know which features of an automated medication dispenser are needed but not know which particular model is appropriate or how it is acquired. Thus, input from finance, IT and pharmacy are critical to selection, procurement and implementation.
Clinical staff can help to identify project-specific factors such as marketing, clinical applications, government regulations, test or procedure volumes, patient demographics and staff preferences. Most importantly, the project team will be sure all equipment and systems meet clinical needs and program criteria.
The planning and cost-estimating process is a precursor to the procurement process and should result in clinical specifics. The more clinical specifics identified in the meetings, the more accurate and manageable the cost estimate. For example, a cost estimate for a 3-D ultrasound for fetal studies requiring five transducers that is based on discussions with the clinical staff is more exact than simply estimating a diagnostic ultrasound. Specifics also can help to identify items that are being added to the project that were not part of the original scope. For instance, the reference to fetal studies might be a red flag that the equipment is beyond the project parameters.
Providing specifics also can help to identify wish list items. However, restraint should be exercised because a construction project sometimes may be viewed by staff as an opportunity to get items they requested in previous capital budgets but were denied. Wish-list items should be considered only after all the medical equipment needed to meet clinical and program goals has been purchased.
Leadership meetings. In addition to clinical input, the team should meet with key leadership to address possibilities of future change in procedures, volume, staff and other variables. Then, medical equipment appropriate to those possibilities can be planned.
Leadership also must understand the impact of timely design decision-making on the overall project budget. Design and construction are based on exact details, and placeholders for fixed equipment don’t provide the necessary level of detail. It is better to design around a specific computed tomography (CT) system and, if necessary, modify the design for an alternative system later.
Managing change
Change orders and specification adjustments are among the key moving parts that health facilities professionals must manage before, during and after a major design and construction project. Medical equipment is easily among the most expensive variables subject to these types of changes.
Reconcilable differences. At some point, a variance may exist between the initial medical equipment budget and the medical equipment cost estimate developed during planning. If the medical equipment cost estimate is less than the initial budget, the project team should not look for ways to spend what may be perceived as extra money. If the medical equipment cost estimate is more than the initial budget, the team should look for ways to reduce the cost estimate. The approach will depend on the magnitude of the variance. Adjustments could require a simple change in manufacturer or model for a specific item or a significant change in the project scope.
Significant discrepancies between the estimate — based on what the users identify as requirements for meeting clinical goals — and the budget may signal a problem. Operational requirements may have changed and the original estimate may have been based on incorrect or incomplete information. Or advanced technology may have resulted in increased equipment costs, which could be offset by operational efficiencies.
Whatever the case, the initial budget and the medical equipment cost estimate must be reconciled before procurement begins. There only should be one set of numbers to track during procurement.
Planning for reuse. The team shouldn’t automatically discard replaced medical equipment. They should look into relocating existing medical equipment, with the caveat that current equipment in good condition at present may be obsolete by the move-in date. For example, a patient exam table that is no longer manufactured but is in good condition is appropriate for relocation. However, an eight-year-old, 16-slice CT scanner that is in good condition may no longer be appropriate for a hospital with a growing emergency department.
Managing to the budget
At the end of the design phase, a procurement schedule should be established based on the construction schedule. Construction delays due to not having the equipment on-site can cost more than the equipment itself. The medical equipment planner and the contractor should coordinate to identify items that are considered critical-path equipment. By definition, this is equipment that can derail a construction schedule if it is not delivered to the job site when the contractor needs it.
Procurement policies and procedures. A successful procurement process that stays within budget involves a collaborative effort, continuous review and reporting of measurable results throughout the life of the project. The end result could mean having money left over to address the wish list in part or in total.
A team and process should be established for clinical review and approval of all items that are scheduled for purchase. This team might include one or two principals, such as the chief operations officer and a department head, who were involved during the design process and are aware of the organization’s ongoing objectives. They must be informed, decisive and responsive to support the construction process.
Clinical input. Clinical review, acceptance and approval are critical before proceeding with any purchase. Circumstances may have changed since clinical equipment first was specified, and a new solution may be necessary. The project team should establish a procedure for approving changes to the final equipment plan. The team must know the variance between the cost estimate and the purchase price before the purchase order is issued.
Settling accounts. If the team has spent less than expected, they must be careful not to spend the savings before all accounts are settled. For every purchase order that is under budget there probably will be one that is over budget. A budget status report, comparing the impact of purchases to the cost estimate and its relationship to the budget should be issued at least monthly by both department and overall project. This document should be required reading for key project stakeholders.
Installation and closeout
Careful planning and management pay off when the project enters the installation and closeout stage, because the project team has created the framework for handling unforeseen situations.
For instance, it is still possible for a piece of medical equipment to arrive on-site and not fit in the area for which it was planned or lack the utilities it requires. If casework must be adjusted, or an outlet must be added for an undercounter refrigerator, a change order or delay may occur. Both may impact the project budget, if not the equipment budget. Fortunately, many of the causes of change orders in the past now can be identified and avoided by using building information modeling.
Another issue during closeout and installation may be building codes requiring certain equipment to be anchored to withstand an earthquake. The responsibility for installation of the equipment may have been established as the vendor or contractor, but the cost of the seismic tie-down kits themselves often come out of the equipment budget.
Ideally, the clinical review, acceptance and approval team, working with the medical equipment planning and procurement consultant and supply chain, will have coordinated to review and approve purchase decisions throughout the procurement process. This coordination will result in no procurement-related design changes and associated change orders.
In addition, a team that has exercised restraint when quotes have come in under budget may enable the organization to purchase equipment that had been deferred earlier in the process or to replace equipment that had been planned for relocation, but is no longer viable.
Best possible outcome
The medical equipment specification, procurement and installation process is fraught with hazards for the project team that does not carefully consider all variables.
Managing change while considering the entire life of a medical equipment project will yield the best possible outcome.
Terry Esquibell and Kelly Spivey are vice presidents at GBA, a health care technology consulting firm based in Franklin, Tenn. They can be reached at terry.esquibell@gbainc.com and kelly.spivey@gbainc.com.
Reduction strategies to align equipment budgets and costs
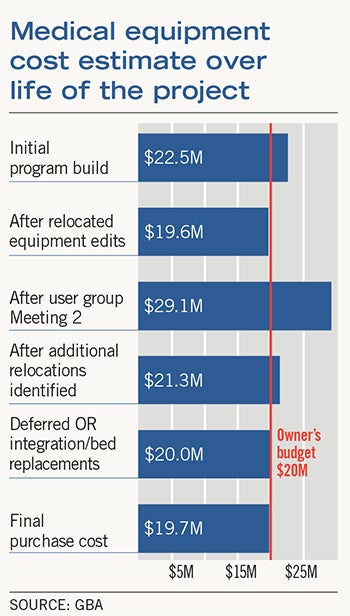
A hypothetical design and construction project can provide several good examples of savings that might be achieved through careful control of the medical equipment specification and procurement process.
One example would be a hospital that embarked on a replacement facility and expected substantial completion in two years. At the start of the project, the facility was in the fourth year of a five-year bed replacement program.
By the end of design, the initial $20 million medical equipment budget (based on 20 percent of construction cost) was $1.5 million lower than the final cost estimate of $21.5 million.
Because additional funding was not an option, the following reduction strategies were identified:
• Purchasing professionals were asked to further qualify the cost estimate with the assistance of the organization’s group purchasing organization (GPO). This identified a potential savings of $225,000 if all purchase orders were placed within the next 10 months. While limitations on cash flow and other factors made this approach impractical, the potential savings from the qualification was still $76,000.
• All departments were asked to reconsider relocating equipment that might be beyond its normal life expectancy but still functioning properly. This resulted in a cost-estimate reduction of $175,000.
• Booms and lights planned for six operating rooms (ORs) remained in the project, but the implementation of OR integration was delayed until after move-in. This saved $600,000.
• The replacement of patient room beds was delayed by two years for a cost savings of $725,000.
These reductions (excluding the potential savings identified by the GPO of $76,000) lowered the cost estimate to $20 million, keeping it in line with the original budget for medical equipment.
The owner had to relocate more equipment than planned and accept delays in bed replacement and implementation of OR integration, but these delays made it possible for the project to move forward.
Establishing an initial medical equipment budget is an important first step. The second step should be developing a detailed cost estimate for medical equipment. This step will determine if the initial budget is in line with the owner’s objectives and identify problems or opportunities that might exist.




