'Code blue'
 An East Coast hospital experienced one of its greatest challenges this summer when a state contractor struck a 30-inch water main, flooding parts of the city and cutting off water supply to others. The hospital was without water, requiring a 2,000-gallon pumping truck from the local fire department to help meet patients' basic needs, including drinking and bathing.
An East Coast hospital experienced one of its greatest challenges this summer when a state contractor struck a 30-inch water main, flooding parts of the city and cutting off water supply to others. The hospital was without water, requiring a 2,000-gallon pumping truck from the local fire department to help meet patients' basic needs, including drinking and bathing.
The International Building Code (IBC) currently requires two sources of incoming water service to hospital buildings to reduce the potential of loss in water supply due to a service main break. This is generally fulfilled by having a municipal water tap enter the building from two separate locations. Beyond this, though, current codes do not require emergency on-site potable water storage, leaving a hospital vulnerable to the same threats as the municipal supply.
The Joint Commission's required emergency operation plan for hospitals includes provisions for emergency generators, the relocation of patients, sheltering and the shutting down of air-handling equipment in the case of chemical attack, but does not clearly address requirements for an emergency potable water system. However, the Centers for Disease Control and Prevention (CDC) and the American Water Works Association have published an Emergency Water Supply Planning Guide for Hospitals and Health Care Facilities (see sidebar on page 37) to assist in planning for a disruption of water and suggesting that health care facilities maintain enough water for eight hours of emergency distribution.
The American Society of Plumbing Engineers' (ASPE's) out-of-print publication, High-Rise Plumbing Design by Alfred Steele, P.E., CIPE, estimates the minimum hourly flow rate of domestic water for a hospital to be 3 gallons per bed, per hour, with an average daily consumption estimated between 235 and 300 gallons per bed, excluding HVAC systems. This means that the average 200-bed hospital in the United States can use as much as 80,000 gallons of water per day. Thus, it is crucial that every hospital have an emergency plan for potable water.
Water planning process
When planning for exterior emergency storage in existing hospitals and during the design phase for new hospital construction, it's important to estimate the minimum flow rate per bed and per hour to determine the amount of water that will be required for an eight-hour period. Also, in both existing and newly constructed hospitals, an estimate of the water required to maintain HVAC systems for the eight-hour period based on reduced cooling in noncritical areas and the fire suppression water storage can be determined based on the National Fire Protection Association's NFPA 14, Standard for the Installation of Standpipes and Hose Systems.
The NFPA 14 code minimum for fire suppression systems is based on the number of stairwells in the building. The engineer must design for 500 gallons per minute (gpm) for the first stairwell and for 250 gpm for all subsequent stairwells, with a maximum of 1,000 gpm for hospitals that are fully sprinklered. If a building is not fully sprinklered, NFPA 14 will max out at 1,250 gpm.
Once the number of stairwells in the health care facility has been determined, the amount of fire suppression water in gallons per minute must be multiplied by the 30 minutes of fire suppression required. For example, a large hospital with five staircases that is not fully sprinklered will require a 1,250-gpm fire suppression system. Adding all this extra water to the building's storage may require additional structural support, thereby increasing costs.
Although NFPA 14 specifies 30 minutes of fire suppression system storage in case of an emergency, it's important to check the hospital's insurance rider as well, because the requirements of insurance carriers can be above and beyond the code minimum.
Planning for existing hospitals. The first step in planning emergency storage within an existing hospital is for the building's facilities team to use current meter readings to determine how much water is being used on a daily basis. Subsequently, this will be used to determine how much demand can be eliminated or reduced in noncritical areas during an emergency. Some examples of water reduction might include cancelling outpatient procedures, closing laundry facilities and recommending that patients take sponge baths instead of showers. Once this is completed, it can be determined how much potable water is needed.
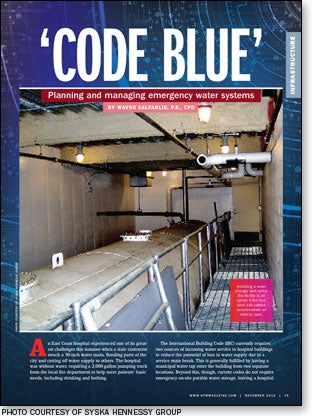
The easiest and most convenient way for an existing facility to add emergency water storage for the first eight hours is on-site at the building's exterior, assuming the site is big enough to accommodate it. If not, a water tank can be placed inside the building but additional structural support may be required, depending on its location within the hospital. Either way, the water from the exterior tank should be connected to the building after first running through a filtration system to clean the sedentary water.
When applicable, two rules of thumb apply:
• The potable water must be replaced every six months to one year, or a water circulating and sanitizing system can be employed to monitor the chlorine reduction levels in the water and add chlorine as needed to maintain potable water quality.
• Existing building pumps must be sized to provide adequate pressure at the top of the building or include a booster pump.
For existing hospitals without exterior or interior water storage capabilities, storing bottled water will be essential. Because it may be impossible to store enough bottled water to cover the full eight hours, such facilities should make sure to plan for an alternate supply of water to kick in sooner.
Beyond the eight hours of water storage, the building must have some means of connecting to an alternate supply of water, like a nearby well, lake or a water truck until the municipal supply returns. This would also require filtration and sanitizing systems to ensure potable water quality, and potentially additional booster pumps if the existing ones are not adequately sized.
If water trucks are going to provide the long-term supply, the building should have a connection point somewhere on its exterior (possibly in the loading dock) so the trucks can connect quickly into the building's pumping system.
Planning for new construction. New hospitals and other health care facilities should consider incorporating emergency potable water storage into the initial design of the building's fire suppression system.
The most likely option is to design a roof tank large enough to provide eight hours of emergency water supply and 30 minutes of fire suppression supply to satisfy both needs. Hospitals should consider using the ASPE water usage estimates along with feedback from the hospital's medical staff to determine how much water storage is needed.
To use water in the upper portion of the tank for emergency water supply, the emergency water supply should be strategically connected above the water level for the fire suppression system so that it is not possible to use the fire suppression reserve water for the emergency supply. This is crucial because the last thing a hospital needs is to have used up the water necessary for the fire suppression system in an emergency.
Again, this will increase the structural steel requirements within the building. If this option is cost-prohibitive, hospitals should consider locating this tank on or below grade. This will eliminate the need for additional structural steel. However, it will require a robust booster pump to distribute the water throughout the building.
Either way, support equipment for any emergency water system, including booster pumps, fire pumps, filtration and sanitizing systems should be placed above the flood level determined by the Federal Emergency Management Agency so the equipment is not affected during a flood. This may mean installing the support equipment above grade, which is prime patient bed space, but crucial to the reliability of the system.

Future water challenges
The biggest challenge to designing emergency water systems in both an existing hospital and new construction is capital cost. Often, these systems can be value-engineered out of a project because they aren't yet mandated by code.
But emergencies like the one experienced by the aforementioned East Coast hospital already provide a strong case for new regulations surrounding emergency water systems, and will continue to push organizations like the CDC, the Joint Commission and the IBC to further develop their existing hospital and health care-specific standards.
The future of emergency potable water systems likely will include the formal issuance of an official code or standard that will mandate water storage for eight hours and beyond. This impending regulation will be based on studies and what the average facility needs; likely will require some sort of quality assurance, especially when using a natural body of water as a potable water source; and will include other health care facilities beyond the hospital, venturing into nursing homes and beyond.
Wayne Salfarlie, P.E., CPD, is supervising plumbing and fire protection engineer and senior associate at Syska Hennessy Group, New York. He can be reached at wsalfarlie@syska.com.
| Sidebar - Water emergency planning advice |
| This year, the Centers for Disease Control and Prevention and American Water Works Association released the Emergency Water Supply Planning Guide for Hospitals and Health Care Facilities, urging health care facilities to establish an emergency water supply plan and describe ways in which a new or existing facility can determine the water required during a municipal water supply disruption. Following is a four-step process adapted from the document that will help any health care facility create an emergency water supply plan: 1. Assemble an emergency service water team. The team should be assembled from a cross-section of departments and the necessary background documents, including contact information, should be collected. 2. Understand water usage by performing a water use audit. Talk to different departments to determine their respective water usage, how much water they need to be stored and which of their services can be put offline or reduced. Some ideas on the facilities side include air conditioning units and boilers; medical equipment such as those used for central sterile operations; medical support equipment such as water-cooled air compressors and vacuum pumps; kitchen equipment such as dishwashers; and laundry facilities. Ideas on the patient side include dietary equipment like drinking fountains and ice machines; pharmacy, radiology and patient room toilets, showers and sinks; lab equipment for running tests, and providing eye-wash and shower facilities; and hazardous materials and decontamination capabilities in the emergency department. 3. Analyze emergency water supply alternatives and decide which are viable. Look at groundwater, surface water, nearby bodies of water, other public water supplies and water supply trucks as well as an on-site bladder tank. (If a hospital has enough notice that the water supply will be disrupted, it can use a bladder tank that can be rolled out on-site for water storage as opposed to a storage tank with a fixed location.) 4. Develop and exercise the plan. Get steps 1, 2 and 3 together and try them out. |




