Planning for energy resiliency
Using generators for load shedding and demand response can provide income to offset the cost of installation and maintenance.
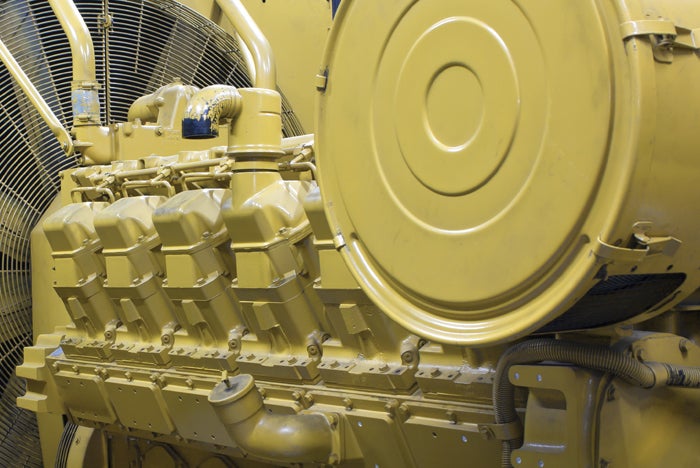
Photo by Shutterstock
The risk of losing grid power as a result of natural disasters and grid failures is increasing and requiring hospitals to consider new ways to support the long-term resiliency and sustainability of their campuses. Adding to the difficulty is the continued pressure to reduce costs to keep the hospital financially viable.
The good news is that a business-planning approach to energy resiliency may create the financial resources to install the needed equipment. For instance, emergency generators are not reimbursed by Medicare and can be a substantial cost. Yet, by using a standardized design and taking advantage of group purchasing leverage, hospitals can substantially reduce equipment, engineering and installation costs. Furthermore, using generators for commercial purposes, including load shedding and demand response, can provide income to offset the cost of installation and maintenance.
Business planning for resiliency reaps cost benefits, environmental benefits and social benefits. Consequently, hospitals will need to adopt financial methods of analysis to begin to view campus-power generation as a worthy investment, create compelling business plans for obtaining financial incentives, and source the know-how, funds and equipment assets needed to ensure the facility’s long-term resiliency.
This requires an integrated, business-oriented approach to energy planning and sourcing as outlined in the American Society for Health Care Engineering’s “Best Practices in Business Planning for Energy Resiliency,” from which this article is excerpted.
Committee planning process
For decades, energy has been the exclusive responsibility of the hospital facility director. Today, professionals from other departments can provide substantial value in energy planning and sourcing.
The best way to obtain the expertise and support necessary for a strong energy-management program is to form a cross-functional team that brings together the expertise of several disciplines within the health system. When seeking the participation of the various members of the energy committee, the following roles should be considered:
- Facility department. This discipline has specific knowledge of the hospital’s energy needs, including equipment, usage and anticipated changes in demand. This critical information will be helpful when deciding whether to make an investment in energy generation on campus. Facility staff will also provide information regarding the relationship between utility and market energy supply and on-site operations.
- Corporate finance. This department manages the institution’s financial investments. Because energy is a financial market, recruiting finance leaders to share their expertise in this area is vital to the success of the endeavor. Equally vital is that finance leaders acquire a fundamental understanding of the opportunities and costs of energy resiliency. Finance is also responsible for managing the institution’s budget, knows how much market risk the institution is willing to take and has a fundamental understanding of financial products.
- Supply chain/purchasing. This department brings to the committee in-depth knowledge about the institution’s purchasing practices. The energy committee will rely on this group’s expertise in negotiating energy contracts and terms.
Key elements of the process
A robust business plan for energy resiliency will take these foundational steps:
- Prepare for emergency conditions. Hospitals should be ready to operate a larger array of patient care operations under emergency conditions for longer periods of time. Recent hospital-resiliency failures have demonstrated that facilities should be prepared to go beyond minimum regulatory requirements and maintain more extensive operations in island mode.
- Allocate resources. Hospitals should allocate resources to resiliency despite continual financial pressure and changing regulatory and market forces. By employing a business-planning approach, facility managers have a greater chance of demonstrating a compelling financial case for investment in energy assets that provide greater resiliency.
- Reduce energy supply costs. Hospitals should view on-campus power generation as a method of reducing the cost of external power supply. This approach should include analysis of how the generating units can reduce the cost of external energy supply, particularly at peak demand.
The primary goals of the energy committee are to conduct a thorough assessment of campus-energy requirements, now and in the foreseeable future, consistent with the facility’s master plan; identify the appropriate energy assets, including on-site power generation and demand reduction, to support campus resiliency and facility equipment life cycles; build a business case for investment, including financial incentives and support; mobilize organizational support; and bring energy initiatives to successful operation.
To be successful, the energy committee must determine the health system’s financial goals and strategic plans for its campuses and whether the existing energy infrastructure will support those plans; determine a loss value for partial or total facility shutdown, including patient revenue, physical assets, brand identity and community goodwill, along with a probability model assessing the likelihood of the losses occurring; determine a value for investment in projects to prevent shutdown; determine whether the health system can or will commit to making the investments necessary to prevent the projected losses; develop a strategic road map for equipment addition, installation and replacement including forecasts of space usage, organizational growth and available incentives; build a business case to fund improvement projects with a cost or payback within a specific range; employ a cost and value-weighting system covering reliability, sustainability and cost management to ensure that limited available funds are used toward projects with the highest weighted value first; rank projects according to value and not according to current staff workloads; define an approval process to fund system improvements or repairs to maintain or improve reliability; and commit to reinvesting energy-
efficiency gains in additional energy-related projects.
Business planning will require certain engineering support and data. In fulfilling its duties, the energy committee should ask the following questions:
- Does the committee have a qualified energy-management engineer to support collection, compilation and analysis of key energy and converted-energy use and cost data?
- Does the energy committee have a qualified engineer to review the resiliency of the supply chain from the point of utility supply to the point of delivery in such critical areas as operating rooms or other critical care facilities?
- Does the committee have a process in place to coordinate major facility changes including expansions, reductions, equipment changes and environment changes with energy use, cost, equipment capacities and impacts on resiliency?
- Is the committee measuring, trending and analyzing key energy and converted-energy supply chains at sufficient intervals to identify trends of inefficiency, reduced capacity and recurrent failure mechanisms?
- Do key decision-makers have sufficient information and understanding of the information regarding energy and converted-energy supply chains, options available, and cost of options, including risk comparisons, to make the best decisions going forward?
- Are these decisions in line with the facility master plan when looking out five to 10 years and beyond?
- Does the committee have a clear vision and understanding and cost weighting of priorities regarding resiliency of energy supply and converted-energy supply?
If the answer to any of these questions is no, the committee should engage engineering and business-planning professionals to support the resiliency process.
The energy committee should be familiar with the facility’s strategic master plan and work toward achieving the stated goals. Energy cost, energy resiliency, energy management and sustainability should be considered part of the plan, including low-cost and energy-efficient infrastructure retirement/upgrade cycles; reduction targets for energy spending and usage intensity; projections of fuel costs and energy spending; continuous service throughout the facility’s life cycle and growth; continuous service throughout unexpected natural disasters; and increased sustainability of energy supplies.
Conducting a needs assessment
A thorough energy assessment should be conducted early in the process to determine system-load requirements now and for any future changes in campus energy load. This should include an on-site assessment of major energy equipment including boilers, chillers, cooling towers, heat exchangers, major air-handling units, generators, electric, steam and hot-water distribution.
To ensure accuracy, the assessment should include installation of electronic data loggers on major equipment for a period of at least two weeks to collect energy-use data at one-minute intervals; use of thermal-image cameras, flow measurements and electrical test equipment; and interviews with operators to gain increased understanding of daily and seasonal system operations.
The evaluation process should include equipment efficiencies and determination of potential operational improvements; cost and savings for projects that would improve reliability and reduce costs; potential of on-site cogeneration; review of all possible energy-
source alternatives, including electricity, fossil fuel, solar, wind, geothermal, battery storage and chilled-
water (ice) storage; investigation of available utility- and government-incentive programs such as rebates, tax incentives, emissions credits and project-financing options; and detailing of current status, potential projects, project cost and expected savings, rebates and tax incentives, and expected timelines.
Once the needs assessment is completed, the hospital will need to choose equipment that correctly fits its on-campus resiliency requirements. For hospitals that have multiple energy alternatives available, the energy committee is encouraged to explore a broad variety of systems that will increase efficiency, reduce cost and provide resiliency.
These alternatives might include solar, wind, geothermal, battery storage or chilled-water (ice) storage, among others. However, the three most common varieties are cogeneration, or combined heat and power, in which a single engine or turbine produces electricity and thermal energy in support of regular hospital operations; backup generators, which are assumed to run only in emergencies or, if Environmental Protection Agency Tier 4-qualified, to run when needed to reduce peak demand; and fuel cells that can provide both cogeneration and backup power without fuel combustion, although currently at a higher unit cost than combustion sources.
Building the business case
A typical scene witnessed in hospitals across the country involves the facility manager having to identify an equipment need, hire engineers to calculate a simple payback and, if the term of years is less than five, present the case to the chief financial officer (CFO) for approval. In too many cases, the CFO rejects the request.
Unfortunately, the facility manager is presenting a case that doesn’t communicate sufficient value to the CFO, and the CFO has many other valuable projects that take precedence, most likely because the other projects generate revenue. To be successful in moving energy projects forward, the facility manager must communicate a better value proposition and do so in language the CFO will readily understand.
Strategies that demonstrate financial value include:
- Calculate using generators to offset utility-demand charges. On-site power generation can earn revenue and reduce hospital energy costs by reducing utility-
demand charges. The utility is permitted to levy a monthly demand charge to recover the cost of providing reliable electricity generation and distribution capacity to customers. Demand charges are a significant source of revenue for most utilities and in many cases can account for more than 33 percent of a hospital’s monthly electricity expense. - Calculate using utility incentives to reduce capital costs. Utility-incentive programs can provide financial resources for planning and sourcing energy-resiliency projects. Many states have created rebate programs as an incentive for hospitals to develop combined heat and power systems.
- Aggregate group purchasing to reduce equipment and service costs. Equipment manufacturers respond favorably to group procurement of energy goods and services. By purchasing multiple generators and service contracts, groups of hospitals can drive supplier margins well below the single-unit rates. Many of these manufacturers also have programs to provide equipment financing.
- Factor in generators as insurance against business losses. Even a short-term power loss can result in a major economic loss for a hospital. Financial losses suffered by hospitals as a result of power failure have included forced closure, canceled surgeries and outpatient appointments, loss of pharmaceutical inventory and, in some cases, evacuation of patients to other acute care facilities. The short-term economic impact can run to millions of dollars. Moreover, avoiding power interruption can potentially help lower overall property, liability and business-interruption insurance costs.
- Take advantage of energy-supplier financing. A number of major energy suppliers and demand-response providers now offer project financing that is rolled into the price of market electricity and natural gas supply or the demand-response contract.
Putting the plan together
The business plan for selecting, financing, sourcing and installing on-site power generation should include the following elements:
- The cost of evacuating the hospital, including both lost patient revenue and damage to the institution’s reputation and standing in the community.
- A thorough energy assessment conducted by a qualified energy professional to determine system-load requirements.
- A comparative evaluation of equipment based on its true resiliency, meaning that multiple-unit generation should generally be preferred over single-unit co-generation.
- The possibility of offsetting the local utility’s demand charges by running generators to reduce peak-load contribution.
- The availability of government and utility incentives.
- Group procurement of multiple generating units to drive down supplier margins.
- Any liability-, property- or business interruption-insurance savings.
- Alternative methods to finance the equipment directly, including equipment-supplier loans or financing on the electricity-supplier bill.
- A competitive sourcing process for the equipment, installation and service.
Addressing energy investments
To ensure optimal energy efficiency and resiliency, it is vital that health systems address energy investments as part of long-term facility master planning. As hospitals embrace the importance of energy investments, they are sending a strong positive message to their communities: “When disaster strikes, we will be here to provide care.”
Mark Mininberg is founder, president and CEO, Thomas Mort is the Saving with Energy and senior adviser, and Steve Jalowiec is vice president of engineering services, at Hospital Energy LLC, Elmhurst, Ill. They can be reached at mark@hospitalenergy.com, tcmort@live.com and sjalowiec@hospitalenergy.com.





