Shades of Green
 Although they are steadily gaining ground, hospitals appear to be inching rather than rocketing down the road to environmental sustainability.
Although they are steadily gaining ground, hospitals appear to be inching rather than rocketing down the road to environmental sustainability.
While the overwhelming majority believes the green movement is truly important for the planet, patients, staff, the community and their own bottom line, hospitals are at various stages of embracing sustainability for reasons ranging from funding and staffing challenges to uncertainty about how to wrap their arms around such a complicated, multilayered issue.
The result is relatively slow growth in sustainability initiatives, according to a 2013 Health Facilities Management survey conducted in cooperation with the American Society for Healthcare Engineering (ASHE) and the Association for the Healthcare Environment (AHE). Although some green initiatives showed a slight increase, most of the 2013 findings were consistent with the results of the previous survey undertaken in 2010 — the first HFM survey on this issue.
 Nevertheless, the path to sustainability is a journey, not a destination, according to experts who are quick to point out that data from the 2013 survey of HFM subscribers, ASHE and AHE members offer much reason for optimism.
Nevertheless, the path to sustainability is a journey, not a destination, according to experts who are quick to point out that data from the 2013 survey of HFM subscribers, ASHE and AHE members offer much reason for optimism.
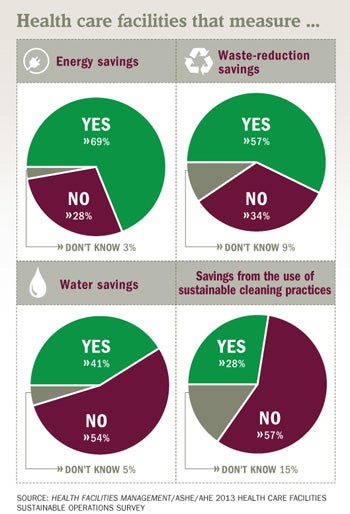
For example, even though the percentage of the survey respondents who said they measure energy savings didn't increase from 2010 to 2013, that number (69 percent) is still significant, experts say.
"If 69 percent of hospitals are continuing to measure their energy savings, that's a huge win," says Tom Thompson, sustainability coordinator at Gundersen Health System, La Crosse, Wis. "There is still work to do, but that's a significant number and we need to look at what we have accomplished instead of at the missing 31 percent."
Despite enthusiasm for the green movement, securing environmental dollars in a still sluggish economy remains a major challenge among respondents who named cost as the top factor influencing whether a facility opts for environmentally sustainable operations.
"Hospitals are dealing with many important issues and there are competing priorities," says Dale Woodin, CHFM, FASHE, executive director of ASHE. "Environmental issues don't always come out No. 1."
Not surprisingly, hospitals are making bigger strides in less cost-intensive areas such as upgraded lighting, which was cited as the single greatest success in a sustainable operations project followed by replacing building automation systems. In terms of waste management, recycling of pharmaceutical/regulated medical waste as well as green cleaning continued to gain momentum in 2013.
But the survey also was revealing in terms of what hospitals are not doing on a wide scale, such as tracking performance metrics. Only 38 percent include performance metrics — such as the Environmental Protection Agency (EPA) Energy Star rating, total waste generation or a recycling rate — in their senior management dashboards and the percentage of those who track energy overall stayed fairly static from 2010 to 2013. For example, less than half (45 percent) of responding hospitals conducted energy audits in 2013 — a drop of roughly 5 percent from 2010.
Considering the close link between metrics and cost-cutting, experts say those numbers need to turn the other direction — quickly.
"Those numbers are shocking," says Janet Brown, director of facility engagement at Practice Greenhealth. "Environmentalism aside, this is also a financial issue, and these metrics let cash-strapped hospitals know where they have opportunities to save money, where they don't and where to prioritize."
Others take more of a glass-half-full view of the survey data. "The EPA would love to see that number grow, but we're happy that so many hospitals have come a long way in a relatively short period of time and are saving tremendous amounts of energy — and money," says Clark Reed, who heads the health care facilities division of the Energy Star program. "Compared with where hospitals were even 10 years ago, this is real progress."
Focus stays on funding
Funding — the need for it and roadblocks to getting it — was a central theme throughout the survey, which was conducted online in March and April by Perception Solutions Inc., Aurora, Ill.
Cost savings was cited as the top factor (84 percent) in determining whether hospitals should pursue environmentally sustainable operations, followed by quality of indoor environment for staff (81 percent), long-term cost benefits and sustainability (80 percent), return on investment (76 percent) and consistent with hospital mission (71 percent).
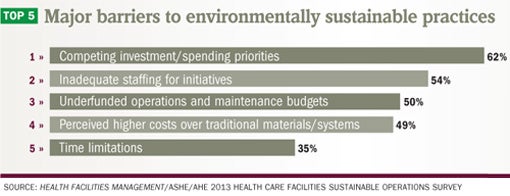
Respondents asked to name barriers/challenges to sustainable operations also cited cost-related reasons most frequently. Competing investment/spending priorities (62 percent), inadequate staffing for initiatives (54 percent), perceived higher costs over traditional materials/systems (49 percent) and underfunded operations and maintenance budgets (50 percent) were named as the main roadblocks to sustainability.
Those numbers reveal something of a Catch-22 for hospitals that often lack the funds to implement the green initiatives that could save them significant money. That's why metrics are so critical, according to ASHE President Mark Kenneday, CHFM, FASHE, vice chancellor, campus operations, University of Arkansas for Medical Sciences, Little Rock, who says that data are vital to gaining a commitment from hospital leadership who also create frequent barriers to sustainable initiatives.
"The key to future success and growth of sustainable operations is by assuring measurement and verification strategies that have the depth and development necessary to measure outcomes going forward," Kenneday says. "Our facilities must benchmark their performance in Energy Star so they can baseline performance prior to energy-efficiency activities, then measure and verify performance over time."
 Hospitals have room for improvement in terms of tracking energy savings, especially considering they are among the biggest users. Although 70 percent are measuring energy consumption, the top two performance monitoring and management initiatives named dipped slightly since 2010 (45 percent conduct energy audits, down from 50 percent in the 2010 survey; 39 percent set and monitor energy budget and performance targets annually, down from 45 percent).
Hospitals have room for improvement in terms of tracking energy savings, especially considering they are among the biggest users. Although 70 percent are measuring energy consumption, the top two performance monitoring and management initiatives named dipped slightly since 2010 (45 percent conduct energy audits, down from 50 percent in the 2010 survey; 39 percent set and monitor energy budget and performance targets annually, down from 45 percent).
"All hospitals should be tracking their energy budgets," says Laura Brannen, EDAC, senior environmental performance consultant, Mazzetti Nash Lipsey Burch, San Francisco, and founding executive director of Hospitals for a Healthy Environment. "Otherwise, that's just money laying on the table."
To that end, experts recommend that facilities access the free tools and resources available via the Sustainability Roadmap for Hospitals www.sustainabilityroadmap.org), which shows hospitals how to implement real-world sustainability projects, enhance existing efforts and share their environmental successes with other facilities. Three American Hospital Association groups — ASHE, AHE and the Association for Healthcare Resource & Materials Management — collaborated on the website.
While designating one position responsible for environmental sustainability would likely aid green efforts, most hospitals aren't yet going in that direction. Just 23 percent said their facility had designated a single title or position with responsibility for sustainability efforts, up from 21 percent in 2010.
Facilities that are investing in those positions are reaping substantial benefits. One example: Tyler Weaver, sustainability coordinator at Children's Hospital of Philadelphia, since 2007, has developed a comprehensive sustainability program that continues to yield impressive results.
The facility is recycling in 28 categories, has reduced its medical waste by 75 percent — saving more than $1 million each year — and achieved a recycling rate of 53.5 percent for fiscal 2013, exceeding its goal of 50 percent. The hospital has composted 75 tons to date since implementing that program in 2012. "A lot of what I did was educate employees who often don't think about what they're disposing and where," Weaver says.
Energy upgrades on upswing
In terms of energy management initiatives, organizations continue to embrace tried-and-true tactics like performing lighting upgrades and building upgrades.
The top-cited practices were transitioning to electronic ballast and energy-efficient lamps and installing LED exit signs (89 percent), installing occupancy sensors or timers (75 percent), upgrades to building controls (75 percent) and technology for plant equipment (73 percent).
One survey respondent notes: "We are using LED lighting and love the $200,000 annual savings."
Although renewable energy practices (solar, biogas, wind, hydro, geothermal) and off-site renewable energy credits (wind, hydropower, solar, biofuel) were among the least-cited initiatives, hospitals are beginning to think in those terms. One hospital is researching wind turbines, another has installed a 50-kilowatt solar system resulting in annual energy savings of $12,000, and another has installed ground source geothermal heat pumps in all new construction since 2001, the survey shows.
More hospitals are embracing commissioning or retro-commissioning — an audit to review building performance of energy systems — on a wider scale, likely because the process brings a return on investment. About 70 percent have implemented commissioning or retro-commissioning, are in the process of doing so or plan to in the next 24 months, the survey shows. One facility cited in the survey used retro-commissioning to decrease utility usage by 30 percent, while another decommissioned a 5-year-old inpatient building, improving its Energy Star rating from 17 to higher than 50 with significant cost savings.
"The only way to ensure getting the most value from your building is to go through the commissioning process, whether it's new construction or an existing building," says Woodin, who recommends hiring a specialist to conduct the audit. "I think it's a vitally important process."
Going to waste
Although hospitals produce more than 5.9 million tons of waste annually, the survey showed a slight drop in measuring waste stream reduction. In 2013, 57 percent measured waste stream reduction, down from 61 percent in 2010.
The drop likely is related to the lack of staff and/or resources available to do the work, which is consistent with the survey's feedback about competing investments and spending priorities, according to AHE staff.
Other commonly cited initiatives were a waste management plan for all materials and waste streams (74 percent), facilitywide management programs (75 percent), tracking waste volume and cost (69 percent), and establishing baseline rates and cost for recycling and all other waste categories (66 percent).
While the numbers are healthy, they should be higher across the board, experts say. "Waste is a measurement of your inefficiency," says Brannen. "If you're not tracking your inefficiency, you're wasting money."
The good news is that there's plenty of help out there. "It's exciting that there are vendors who have become very important business partners for hospitals," says Brown. "They not only remove the material but help with staff training, education, data for tracking and more. Hospitals should have a plan that identifies a vendor."
Although not measured on the 2010 survey, medical waste initiatives scored big in 2013: Regulated medical waste programs were cited by 94 percent of respondents, pharmaceutical medical waste programs by 87 percent, and reusable/recyclable sharps by 68 percent.
"Reprocessing of single-use devices should be a no-brainer," Brannen says. "There are still a lot of perceived barriers, but facilities that get past them are saving millions."
Waste water?
Hospitals aren't yet making great gains in water conservation, but they are starting to take a closer look at it. "Water is going to be the next big thing," Brown says. "There are tremendous opportunities in everything from recycling dishwater, to monitoring water use, to just using efficient dishwashers and low-flow fixtures."
The percentage of hospitals that measure water savings stayed consistent at roughly 41 percent from 2010 to 2013, while the most common water conservation initiatives cited in 2013 were low-flow fixtures for toilets and urinals (68 percent), condensate recovery systems (52 percent) and flow-control fixtures on faucets, such as motion sensors (64 percent).
Conducting a water use audit (cited by just 38 percent of survey respondents) is the first step toward realizing potential savings, which can be substantial, says Brown.
Water conservation can yield a return on investment ranging from 25 to 40 percent, which for large facilities can translate to more than $100,000 per year savings in water, sewer and energy costs, according to Practice Greenhealth. One facility in the survey saved 30 percent on its water bill by installing low-flow toilets and urinals, low-flow aerators and removing unnecessary toilets and sinks.
Clean and green
Although just 28 percent of facilities measured savings from environmental cleaning practices (down from 30 percent in 2010), hospitals continue to place a high priority on providing healthy, safe environments and improving the toxicity levels of the cleaning chemicals and air quality.
The survey showed that: 92 percent use microfiber mops, which conserve water; 84 percent use prediluted disinfectant systems for worker safety; and 88 percent use cleaning equipment that doesn't negatively impact indoor air quality. Those figures are driven by cost savings, quality of environment for staff, patients and visitors, and alignment with the hospital's mission, according to AHE staff.
Brown also lauds the 73 percent who cited installation of sustainable floor care materials. "When you talk to hospital staff about what makes them feel sick, waxing and stripping of flooring materials are often the first thing they mention, so this is really important," Brown says.
Recycling rates remain high among standard items — cardboard (89 percent), paper (78 percent), batteries (77 percent), beverage containers (69 percent) and metal (63 percent) — and are also beginning to take hold in areas like e-waste (48 percent) and construction debris (41 percent).
"Construction and demolition debris present a good opportunity for recycling since they make up the biggest component of landfills," Brown says.
One facility recycled 90 percent of its debris during recent construction of a new facility, according to the survey.
Future looks green
Down the road, Woodin says a likely uptick in the construction industry could boost environmental sustainability initiatives at hospitals. "Construction has been very slow in hospitals, and as it starts to pick up, CEOs will begin to make capital purchases like sustainability projects."
In the interim, he urges facility and environmental services managers to keep upper management informed of their current success. "It's really important to take credit for good work that's been done so that you can ask for additional funding," Woodin says. "That's what gets you to the second and third level of projects."
All experts contacted for this report urge hospitals committed to green initiatives to embrace the rich supply of resources available to help them gain ground.
For hospitals that aren't sure where to begin, Thompson recommends starting with Practice Greenhealth and the Healthier Hospitals Initiative, which not only offer a litany of tools and resources, but connect users with others on the same path. And the Sustainability Roadmap for Hospitals provides free, practical tools to help health care facilities reduce their environmental footprints.
"These groups need to keep spreading the word, educating health care and leading by example," Thompson says. "Although each facility is unique, the challenges are pretty universal."
In the meantime, hospitals continue to make progress one project at a time. One survey respondent says: "We are taking baby steps along the way to improve our operations. Even though our organization has not embraced sustainability as a cultural mindset, our facilities management group continues to make progress despite tough and uncertain times in our industry."
Beth Burmahl is a freelance writer based in Oak Park, Ill., who specializes in health care topics, and Suzanna Hoppszallern is senior editor of data and research for Health Facilities Management's sister publication, Hospitals & Health Networks.
| Sidebar - Hospital sustainability projects run the gamut |
| Although hospitals appear to be going green gradually, many are scoring significant energy savings through a growing roster of sustainable initiatives that are helping to reduce their carbon footprints. "Hospitals are starting to find their opportunities for sustainability projects," says Tom Thompson, sustainability coordinator at Gundersen Health System in La Crosse, Wis. "Some of these projects might not be what you would call exciting — like scheduling air handling units on the roof of our clinic — but there are significant savings to be had even if these projects aren't grabbing headlines. The real work is done on the front lines of facilities management." Hospitals across the country are exploring new — even creative — green territory along with continuing to embrace the initiatives that are proven cost- and energy-savers. Following is a sampling of health system initiatives under way, based on responses to the Health Facilities Management/American Society for Healthcare Engineering/Association for the Healthcare Environment 2013 Sustainable Operations Survey. Energy• An LED project under way at Maury Regional Medical Center in Columbia, Tenn., is saving the hospital about $12,800 per month with a 30-month payback using Tennessee Valley Authority and state grant money, says Paul Corvin, director of plant operations. The 500,000 square-foot facility also hired consulting engineers who steered the hospital toward similar or higher savings with HVAC system changes. "In March we had a total electrical savings of $37,000," says Corvin, who adds that the changes will be most effective in spring and fall. • A multiphase, campuswide effort at a Pennsylvania-based academic medical center focusing on increasing the building system's efficiency between 2009 and 2012 yielded energy savings of approximately $1.5 million. The third phase is expected to save another $400,000 annually. The facility also reduced its carbon footprint by 11,015 metric tons of carbon dioxide, among other savings. • The University of Nebraska Medical Center is in the process of converting all major systems to digital control, allowing the facility to monitor and trend energy usage, saving millions of dollars. The facility also received an electric company rebate check for more than $1 million, says Dan Murrell, zone facility manager. "There are still other savings to be reaped by these modifications, but they are paying for themselves." • Other energy initiatives mentioned by respondents include installing combustion modulation controls on existing natural gas, low-pressure steam boilers, a retro-commissioning project that reduced usage by 900,000 Kwh and upgrading controls on a new central chiller plant to monitor and reduce energy by 30 percent. Waste• Northwest Hospital Center, Randallstown, Md., increased its recycling percentage from 20 to more than 33 percent over four years and has completed several LED replacement projects and installed an electric car charging station on campus. • "Our OR and facility management teams are both sustainability stars," says Dana Slade, sustainability manager, HealthPartners, Bloomington, Minn., where the OR has implemented greening processes including reusable suction systems, reprocessed equipment and blue wrap recycling. "The team has done some amazing upgrades and worked with our service providers to obtain more than $250,000 in rebates and saved more than $300,000 with our greening the OR initiatives," Slade says. • A blue wrap recycling program at The Miriam Hospital in Providence, R.I., has diverted more than 3,000 pounds of blue wrap from the general waste stream. Mercy Health System works with community law enforcement in Milton and Janesville, Wis., to provide drug drop boxes at several Mercy locations for safe and confidential medication disposal. • Other waste initiatives cited by respondents include using food waste dehydrators, adding a single-stream recycling program and using a waste management system in the OR to eliminate the bulk of fluids going into the medical waste stream. Water• Asbury Methodist Village, in Gaithersburg, Md., developed a successful water-reduction program using a self-created dashboard. Separate water metering for the laundry yielded an annual reduction in water consumption of 702,000 gallons in 2012, while netting a $21,400 savings in water, sewage, gas and chemicals. • Sky Lakes Medical Center in Klamath Falls, Ore., is in the latter stages of a $2.7 million dollar energy program including energy-efficient lighting (LEDs, T-8 ballasts and tubes), new cooling towers, pumps, motors, chiller optimization, controls and commissioning. Expected savings on energy bills is 27 percent. • Other water initiatives respondents reported include installing a rainwater capture system for chiller plant make-up water and using a condensate return system, saving approximately $27,000 annually. Green Cleaning• Somerset (Pa.) Hospital uses a bleach-free laundry program, reducing toxic chemicals in the waste stream. "Where possible, we reduced this dilution rate by almost 75 percent, cutting our cost, the high pH of the discharge water, and maintaining quality," says Bill Tresise, director of environmental services. • Other cleaning initiatives mentioned include switching to microfiber cleaning materials, which saved one hospital 40 percent on housekeeping chemicals; using a cost-saving chemical dispensing system; and using green products such as vinegar to help with the facility's hard water. |
| Sidebar - About this survey |
| Health Facilities Management (HFM), the American Society for Healthcare Engineering and the Association for the Healthcare Environment surveyed a random sample of 4,660 hospital executives to learn about trends in sustainable hospital operations. The response rate was 15.1 percent, or 705 completed surveys. HFM thanks the sponsors of this survey — Amerinet, Georgia-Pacific, Grainger and Mitsubishi Electric Cooling & Heating — for underwriting this research. |




