Air filter selection and COVID-19

Some health care facilities will install HEPA filters in the critical space air-handling units as well as inline ductwork in operating rooms and in AII room exhausts.
Image courtesy of ASHE
When health facilities professionals protect their health care workers, they protect the public. Toward that end, hospital HVAC systems play an integral role in limiting the transmission of infectious diseases to other patients, health care staff and visitors.
The HVAC system is by no means the only safeguard to protect doctors and nurses from getting infected; the role of the appropriate personal protective equipment (PPE) is extremely important in providing the first level of defense. But an enhanced HVAC system design will minimize the recirculation of COVID-19-contaminated air in the hospital air distribution system.
As facilities professionals continue to learn more about the means of transmission of COVID-19, the design engineer and facilities engineer will need to work together to ensure that the modified hospital engineering systems are able to perform effectively to minimize the risk associated with nosocomial transmission of the coronavirus.
‘Airborne precaution’
On March 16, 2020, the World Health Organization put out an “airborne precaution” for medical staff after a new study showed that the coronavirus can survive in the air in some settings. The study showed that the coronavirus can go airborne and stay in the air depending on factors such as heat and humidity. This is on top of the fact that was already known about the coronavirus being transmitted through droplets, mostly via sneezing or coughing. This means that the coronavirus can become aerosolized under certain environmental conditions.
An aerosol is a wholly different physical state; particles are held in the air by physical and chemical forces. Fog is an aerosol in which water droplets are suspended in air. The suspended particles remain for hours or more, depending on factors such as heat and humidity.
If virus particles adhered to droplets of mucus or saliva can be suspended in air for more than a few seconds, as the measles virus can, then anyone passing through that pathogenic cloud could become infected. There are strong reasons to doubt that the new coronavirus has anything close to fog-like capability, but because there is no surety, engineers will need to consider the impact on the air distribution system within the hospital.
“We’ve seen no evidence that aerosolized virus is the primary transmission risk for everyday people in everyday settings,” says Dylan Morris of Princeton University, a co-author of the study on the aerosolization of the coronavirus. “One should not rule anything out categorically with a novel, still-poorly-understood virus, [but] based on what we know about coughing and sneezing, one should be cautiously optimistic that aerosolization may not play a big role in everyday transmission.”
This simply means that facilities will need to pay great attention to ensuring that the air systems are modified to minimize the circulation of the COVID-19 virus in hospital air systems.
Controlling infection
A virus is a small infectious agent that can replicate only inside the living cells of organisms. Most viruses are too small to be seen directly with a light microscope. Viruses infect all types of organisms, from animals and plants to bacteria.
The most important virus in the current pandemic is the novel coronavirus, known as SARS-CoV-2. This is a new coronavirus that had not yet been previously identified. This is not like other coronaviruses that commonly circulate among animals. Coronaviruses from animals rarely affect humans like the SARS-CoV-2 virus.
In recent times, other coronaviruses have caused more severe diseases, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). However, there are many types of coronaviruses in humans that usually cause mild respiratory illness.
Mechanical ventilation systems are part of the mechanism for controlling airborne infection in the hospital environment. The goals of ventilation systems are to replace contaminated air with clean air, to minimize the mixing of dirty and clean air, and to regulate ambient temperature and humidity to help with asepsis and odor.
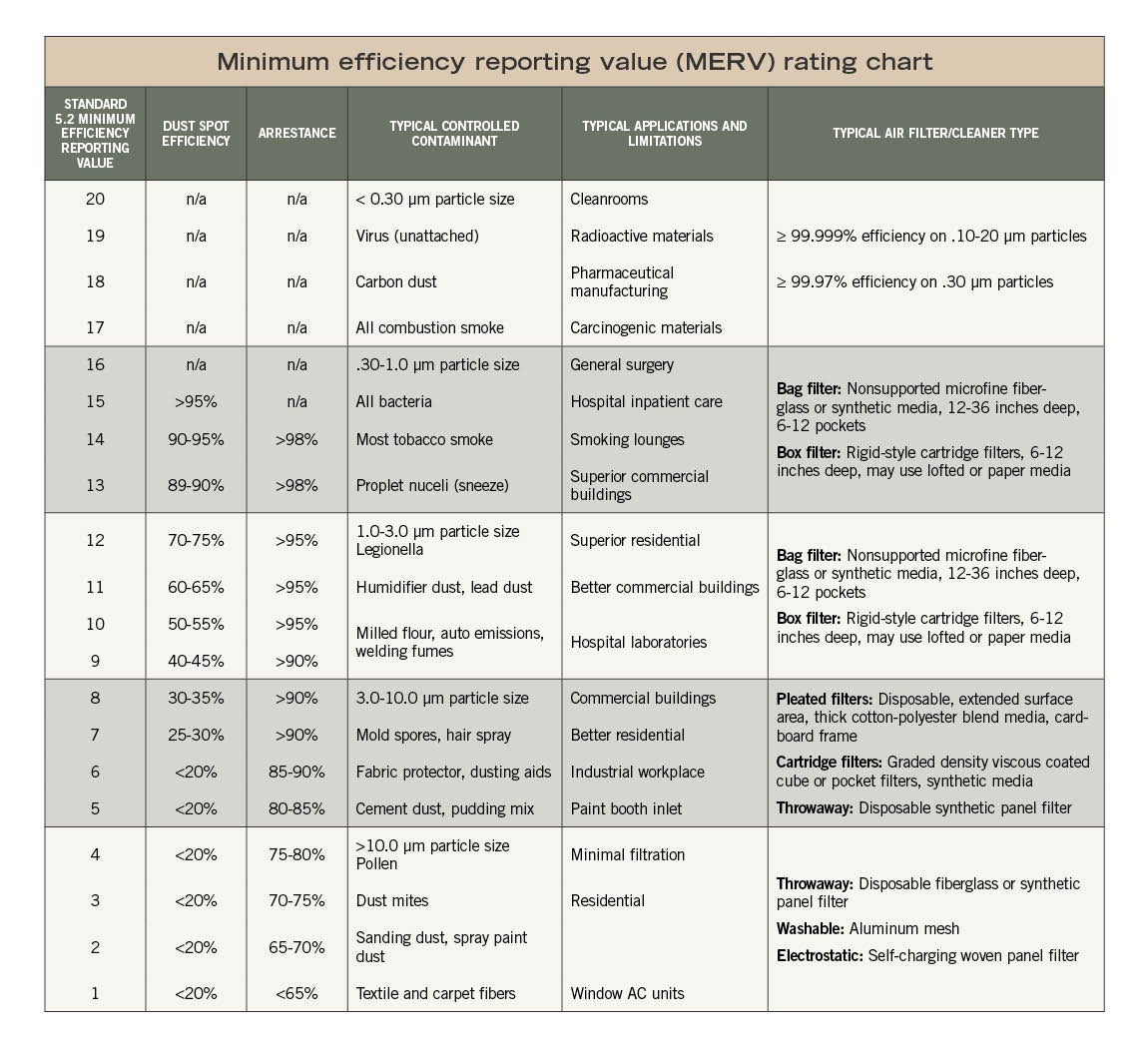
The minimum filtration requirement is mandated by the American National Standards Institute (ANSI)/ASHRAE/American Society for Health Care Engineering (ASHE) Standard 170-2017, Ventilation of Health Care Facilities, for specific filter efficiencies for all the spaces in the health care environment.
Table 7-1 in the updated Addendum p to the standard stipulates the minimum criteria that an air filtration system should meet in health care facilities. The table illustrates the air filtration requirements for the air-handling units (AHUs) that handle most of the airflow within the hospital space. The critical spaces in hospitals are usually fitted with MERV-14 filtration. The table to the right shows that the filtration level of MERV-14 will not be effective in totally removing viruses from the air stream in the hospital HVAC system.
Table 7.1 in Addendum p shows that high efficiency particulate air (HEPA) filtration is only required for protective environment (PE) rooms and combination airborne infection isolation (AII)/PE rooms. However, ANSI/ASHRAE/ASHE Standard 170-2017 are only minimum standards, and some health care facilities will install HEPA filters in the critical space AHUs, in inline ductwork in operating rooms, and in AII room exhausts.
Types of filtration
Air filters are rated based on the size of particles they are able to remove. Filters remove particles from the air stream by intercepting particles that come into contact with the surface of the filter media. A closer look at these filters includes:
Pre-filters. This filter is usually the first level of filtration in an AHU that is installed in a hospital air distribution system. This can vary in MERV rating from 8 to 9. Filters with lower MERV ratings are fairly cheap and impose only a small pressure drop penalty through the air system.
Final filters. This filter is usually the second level of filtration in an AHU that is installed in a hospital’s air distribution system, usually a minimum of MERV-14.
HEPA filters. HEPA filters are commonly used in health care settings’ surgical suites, protective environments and isolation rooms. HEPA filters are ideal for very small particles, measured in micrometers or microns (μm).
In 2005, the Department of Energy defined a HEPA filter as having a minimum efficiency of 99.97% at a test aerosol diameter of 0.3 μm. Although the use of HEPA is not mandatory, it is best practice for engineers to specify these for critical areas in hospitals.
Since the onset of the COVID-19 pandemic, many health care facilities’ air distribution systems have been retrofitted to have HEPA filtration with the intent of capturing and inactivating the SARS-CoV-2 virus. Many of those installations involve placing HEPA filtration on exhaust to ensure that air is not dumped to the external atmosphere without being properly filtered to remove the virus and to minimize the impact on the areas adjacent to the hospital.
The real question is: Can HEPA filtration remove the COVID-19 virus from the air system? The family of coronavirus virus is 0.12 μm, according to the National Library of Medicine. The Environmental Protection Agency also defines HEPA filters as having a minimum efficiency of 99.97% at 0.3 μm.
With this description, there is a misconception that HEPA filters do not remove particles smaller than 0.3 μm. However, HEPA does not act like a strainer where particles above a certain size are not able to pass through; rather, it uses four different filtration mechanisms to trap particles of varying sizes effectively (sizes both larger and smaller than 0.3 μm).
The diameter specification of 0.3 μm responds to the worst case, the most penetrating particle size (MPPS). Particles that are larger or smaller are trapped at an even a higher efficiency; most of the small particles, like the SARS-CoV-2 size, are captured by diffusion.
At this time, there is not direct research to verify if HEPA filtration reduces transmission of the SARS-CoV-2 virus. More validation is needed to determine the efficacy of HEPA filtration on the virus when installed in the HVAC system.
Additionally, for the SARS-CoV-2 virus to travel in the air, it must lodge onto liquids/mucus through coughing or sneezing, which increases their sizes to greater than 0.5 μm to 3 μm. Source control is important to ensure that some of these particles that remain in the air are not entrained into the air distribution system.
This is the main reason why health care systems are using temporary HEPA installations as means of protection for the hospital patients and staff.
Using HEPA filtration
Because it’s known that the primary transmission of the SARS-CoV-2 virus is through droplets, using basic HEPA filtration thus far provides the best means of intercepting the virus before it is spread to the air system.
Installation of HEPA filters on the return and exhaust air systems is the current best practice approach of intercepting the path of the virus in the health care setting. A discussion of these applications includes:
HEPA on exhaust. Installation of HEPA in air exhaust will ensure that the air that is released to the outside is properly filtered and will minimize the impact on the surrounding areas of the building. This is also important to ensure that contaminated exhaust air is not entrained in supply air intake louvers.
HEPA on return (relief). During the first surge of COVID-19 response in hospitals, mechanical engineers worked with facilities to convert AHUs to operate with 100% outside air where possible. This single pass was able to provide the most protection for the hospital staff and patients. The best practice is to ensure that HEPA filters are installed on the exhaust of the AHU. This will allow the facility to protect people who are in the vicinity of the exhaust air to the outside.
HEPA fan filter units. Some installations of AHUs will not allow facilities to retrofit the unit with HEPA filtration. This is often because the units were not designed to deal with such a large pressure drop, the filter section is not large enough to be retrofitted with HEPA filters and also because of the long duration of disruption to the hospital operation if the AHUs have to be taken out of service. The most innovative way of modifying these systems is to install HEPA filter fan units and close off the return air diffusers in the COVID-19 patient areas.
It is extremely important to ensure that the HEPA fans or the closing off of returns do not impact the operation of the AHUs. Installing the fan units closer to the rooms that are near the AHUs will help the system’s stability.
AII rooms. AII rooms were the most sought-after spaces in a hospital during the first phase of the COVID-19 pandemic. This is because negative-pressure AII rooms are used to isolate a patient who is suspected of having an infectious disease such as COVID-19 or has been diagnosed with it.
The AII room is designed to help prevent the spread of infectious disease from an infected patient to other persons in the hospital setting. These rooms protect the health care staff and will continue to be in high demand until a vaccine is found. These rooms are the best spaces for the intubating of COVID-19 patients before they are placed on ventilators and extubating them when they are taken off or other aerosol generating procedures are performed.
Ideally, the exhaust discharge from an AII room should be passed through a bag-in/bag-out filter housing with pre-filters and HEPA filters before it is discharged to the outside. The Centers for Disease Control and Prevention recommends that the fans’ discharge from these isolation rooms should be labeled as contaminated air.
Many health care facilities were able to modify existing patient rooms into negative-pressure rooms for the initial COVID-19 surge. ASHRAE and ASHE released several recommendations of how to convert these spaces into temporary negative-pressure rooms. It is very important to note that these modified patient rooms are not true AII rooms, but they can serve the purpose of source control.
A medical-surgical patient room is required to have fewer air changes per hour than an AII room. ANSI/ASHRAE/ASHE 170 recommends a minimum air change rate of 12 for AII rooms and 6 for normal patient rooms. However, the most important aspect of converting these rooms is to ensure that they have a negative-pressure relationship to the corridor and thus can provide added protection for the staff and other patients in the hospital.
Best practice
Based on the reviews from multiple health care facilities after the first COVID-19 surge, the addition of HEPA filtration to the HVAC is the current best practice engineering approach for protecting patients and staff. However, care must be taken to ensure that the addition of HEPA filtration to the HVAC system does not negatively affect the overall air system performance.
There are other, unproven means of enhancing the HVAC system to protect the staff and patients, such as increasing air change rates (which is energy intensive), operating the AHUs in 100% outside air mode, and converting COVID-19 patient rooms to be negative to the corridor.
There is more work needed to fully analyze the right combination of HVAC solutions that will eliminate the COVID-19 virus from the air system if it is determined to be transmitted via aerosolization, and there needs to be independent studies done to validate the solutions that were implemented as short-term measures so far.
Gary Hamilton, PE, LEED AP, is senior vice president for WSP, based in Montreal. He can be contacted at Gary.Hamilton@wsp.com.