2021 Hospital Construction Survey

When COVID-19 first hit the U.S. like a wrecking ball in early 2020, hospitals were among the most affected.
Faced with a huge surge in patients infected with an unknown life-threatening virus, hospitals took immediate action to keep patients and staff safe while quickly moving to adapt to structural needs that were changing by the day.
Relying on long-standing disaster and emergency preparedness plans and continually updated resources from the American Society for Health Care Engineering (ASHE), facilities staff quickly launched innovative solutions.
“We weren’t as prepared for this type of crisis as we thought we were, but if hospitals had not been focused on emergency preparedness as we have for the last decade, we wouldn’t have been prepared at all,” says Chad Beebe, AIA, CHFM, FASHE, deputy executive director at ASHE.
From day one, facilities focused on critical issues like upgrading ventilation, creating isolation rooms, expanding emergency departments (EDs) and building temporary structures to handle patient overflow.
But, because hospitals had to redirect resources to COVID-19-related issues, many facilities had to put the brakes on other construction projects while they reassessed the situation.
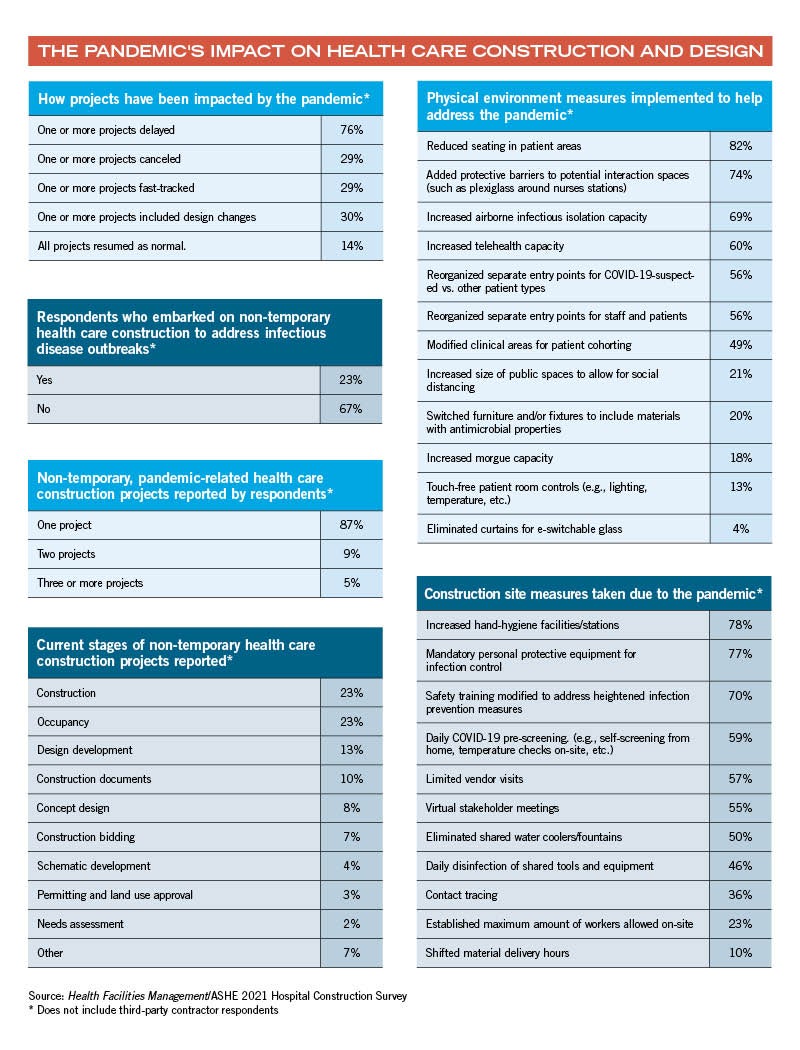
In fact, the vast majority of hospital construction projects were impacted in some way by the pandemic, according to the 2021 Hospital Construction Survey conducted by ASHE’s Health Facilities Management magazine, which included responses from more than 300 facilities professionals at hospitals across the country.
The survey showed that 76% of respondents have delayed one or more construction projects due to COVID-19, while 29% have canceled at least one project altogether. For projects started before the pandemic, renovation was overwhelmingly the main project delayed, canceled or fast-tracked. During the pandemic, renovation is also the main focus, the survey shows.
Pandemic dictates construction
Of hospitals that continued with at least one project already underway, 29% say the project was fast-tracked due to the pandemic.
About this survey
SPONSORED BY
The American Society for Health Care Engineering’s Health Facilities Management (HFM) magazine surveyed a random sample of 7,547 hospital and health system executives, and health care design and construction professionals, to learn about trends in hospital construction. The response rate was 7.3%. The main article focuses on health care organizations and the sidebar focuses on third parties. HFM thanks the sponsors of this survey: Gordian Inc., Greenville, S.C., and W.W. Grainger, Lake Forest, Ill. 
“If the project is already approved and the contract signed, many hospitals will put the project on the fast track and quickly integrate new features like flexibility and modular components to aid during COVID-19 and to prepare for the future,” says Joe Sprague, FAIA, FACHA, FHFI, senior vice president and principal at HKS Architects, Dallas, and a member of the ASHE Board.
Survey respondents who gave anonymous input fast-tracked projects including adding isolation rooms, upgrading/replacing HVAC systems and renovating/expanding laboratories. One respondent added a portable morgue unit.
Said one: “We had a nursing unit renovation that kicked off just prior to the pandemic. The shop drawing process was expedited, and everything that could be fast-tracked for the project was.”
Hospitals also modified designs already underway — often on a piecemeal basis.
One facility updated systems in two older hospital wings to accommodate inpatient surge. Another created an ED triage with quick, pop-up capacity, and another hospital added telehealth to a floor designed with the capability to switch on-demand to provide negative pressure for infection prevention.
Said another: “We added much more mechanical ventilation than the code requires, as well as opportunities for natural cross-ventilation, and we may incorporate operable windows.”
Many hospitals erected temporary structures for short-term solutions made possible by Centers for Medicare & Medicaid Services (CMS) waivers.
“In Georgia, many systems here used the CMS 1135 waiver for temporary structures and built or erected facilities under the national emergency declaration in order to handle patient overflow because of COVID-19,” says Patrick Rhinehart, CSP, CHFM, an environment of care/life safety system manager at Northside Hospital, Atlanta.
While resiliency has long been a staple of hospital design, most construction projects now underway are laser-focused on flexibility, adaptability and potential for the future, Sprague says.
Hospitals that invested in features like modular design pre-pandemic saw a significant return on their investment during the crisis, he says.
“Modular design is very popular, and for good reason,” Sprague says. “You are able to change the function of the room. Let’s say you have a dozen modular rooms in the ED; you assign six to COVID-19 and adapt those with the necessary ventilation.”
One respondent converted a medical-surgical patient floor into a COVID-19-only floor with 100% outside air, exhaust and negative pressure. “This will easily be converted back to a medical-surgical room when COVID-19 is not an issue.”
Planning for the future
While COVID-19 has impacted hospital construction across the board, the survey shows that hospitals are still planning for the future even if their present situation is uncertain. Nearly a year into the pandemic, 33% of health care respondents are moving forward with a permanent construction solution related to COVID-19.
In line with earlier trends, hospitals continue to focus primarily on renovation versus new construction and outpatient versus inpatient projects. Funding will go primarily for building or planning acute care and specialty facilities, medical office buildings, physical plants and ambulatory facilities, the survey shows.
The trend toward microhospitals — small-scale inpatient facilities that offer a wide range of medical services, often in underserved communities — continues, the survey shows. Numbers are rising as hospitals begin to fully understand the concept of microhospitals and how they are reimbursed, says Beebe.
In terms of adding or modernizing specific departments, hospitals are investing less in projects across the board — at least for the time being — as a response to COVID-19.
“Hospitals are making do with what they have in a situation with so many unknowns,” Beebe says. “It’s the same in other fields. Why would a restaurant go through a major remodel when they don’t know what the future holds?”
The survey shows a significant drop in pharmacy departments currently under construction, from 17% in 2019 to 8% in 2020.
Hospitals may have pulled back from pharmacy construction due to a recent postponement of an update in the United States Pharmacopeia (USP) General Chapter 797 regulation for compounding of sterile preparations, according to Jonathan Flannery, MHSA, FASHE, FACHE, senior associate director of advocacy for ASHE.
“There was some uncertainty during the most recent standard development process, so hospitals may have put pharmacy projects on hold until this is worked out,” Flannery says. “After this is finalized, hospitals will know exactly what they will need to do and should start jumping back into pharmacy projects.”
While the survey shows that current construction on non-freestanding EDs dropped by half in 2020, the explanation likely isn’t COVID-19-related. “As we are able to develop more freestanding, urgent care facilities, the burden on EDs of lower acute care emergencies will hopefully continue to go down, allowing EDs to focus more on the high-level acuity emergencies,” Flannery says.
In the survey, many respondents mentioned ED expansion and modifications related to the pandemic, which will likely be reflected in 2021 data.
Ventilation projects soar
In a year that hinged on infection control, it’s not surprising that ventilation projects jumped considerably in 2020. Roughly 46% of respondents are replacing/upgrading or plan to replace/upgrade air handlers and ventilation systems in the next two years. Another 17% are currently replacing or upgrading exhaust fans.
“Ventilation has always been extremely important in health care, but hospitals really had to step up and improve their systems in every way possible during COVID-19,” Flannery says. “After this, we’re never going to look at ventilation in health care facilities the same way.”
The survey shows hospitals are also focusing on replacing/upgrading electrical switchgear/transformers, chillers, and plumbing fixtures and piping.
Hospitals continue to increase their investment in network infrastructure and wired data infrastructure to stay on top of continually advancing technology and connectivity.
“Technology will never stop improving, so hospitals are continually investing in upgrades,” Flannery says. “For example, patients can take their own EKGs from a cellphone now. The possibility of integrating this type of information into a hospital’s data systems so doctors can better monitor patient health could have significant implications for network infrastructure.”
Looking at budgets
Despite having an extremely turbulent year, capital budgets were roughly in line with last year’s numbers. The survey shows more than half of recently completed projects were finished on time or ahead of schedule and on or under budget in 2020. Budgets will remain roughly the same in 2021, the data shows.
But another 24% reported being on or under budget but behind schedule, which can be linked to the construction delays hospitals experienced during COVID-19, Beebe says.
As far as what hospitals are actually spending versus budgeting, there is a slight but consistent downward trend in terms of spending over the past decade. Beebe says this happens as unexpected expenses come up and hospitals look to capital budgets as “low-hanging fruit.”
“Hospitals have a slim operating margin and no real way to generate more money,” Beebe says. “For example, if Starbucks sees their fall sales are low, they can put out a new pumpkin spice latte to generate additional revenue. Hospitals can’t do that.”
Successfully adapting
While the true impact of COVID-19 remains to be seen, hospitals that successfully adapted, modified and developed solutions under enormous pressure had a significant impact on patient outcomes during the once-in-a-century crisis.
Many relied on new resources, guidelines and frequent updates from ASHE to safely implement creative, innovative projects that literally saved lives across the country.
One hospital converted a vacant Sears auto shop into a seven-bay drive-thru lab site primarily used for COVID-19 swabbing, but also for blood draws and other lab exams to reduce entry to the building.
Other survey responses included:
- “With careful infection control measures, personal protective equipment and daily screenings, our team was able to complete a renovation project to an occupied independent living senior care facility that commenced just as the virus was forcing mandatory shelter-in-place protocols.”
- “Engineers offered free design options for turning regular patient rooms into temporary isolation rooms without major construction.”
- “My team was able to make 50 standard patient rooms into temporary negative pressure rooms in a week’s time frame in preparation for a surge.”
Other hospitals also:
- Expedited schedules to open portions of in-progress additions in phases, providing earlier access to patient beds.
- Rolled out mobile telehealth carts to aid inpatient care.
- Added a drive-thru building with a small office used for COVID-19 screening in the parking lot.
- Adapted a new oncology building to accommodate patients solely by eliminating waiting room furniture and adding triage desks at the front door.
Because so many projects were successful, hospitals quickly realized they had long-term potential beyond COVID-19 and plan to keep and/or adapt them for other uses, the survey shows.
Hospitals plan to keep changes, including design changes such as touch-free patient room controls and increased airborne infectious isolation capacity, as well as construction requirements including virtual stakeholder meetings, mandatory personal protective equipment for infection control and contact tracing, the survey shows.
Rhinehart says hospitals should also have an eye toward transitioning temporary facilities built during COVID-19 to permanent buildings, provided the proper regulatory agencies are involved.
“We added 88 beds for COVID-19 observation and, because we included our local, city and state authorities having jurisdiction, we should have no problem keeping the additional beds after COVID-19,” Rhinehart says. “This is now new revenue coming in.”
And ASHE, which assembled a team of infection prevention, construction, safety and other experts during COVID-19, will maintain the team to address a range of post-pandemic issues, Flannery says. “This will be an ongoing effort. It became a great process that was truly effective.”
‘Future is bright’
Based on the impressive response of hospitals to such an overwhelming, worldwide crisis, experts are optimistic about any challenge on the horizon.
“I think the future is bright,” Sprague says. “Health care facilities and the health care design community have been up to the challenges of COVID-19 and, as we view the hospital of the future, we will be better prepared for unknown conditions. The communities and the populations these hospitals serve will be well-rewarded for [the health care field] being on top of this situation.”