Managing for the unexpected

Comparative analytics is an important concept to align scarce resources to optimize the built environment.
Image by Getty Images
The public health crisis of the COVID-19 pandemic and the natural disasters of 2020 have highlighted the ever-present dedication of health care providers who rise to the challenge of maintaining first-class patient care.
Health care teams are community heroes in times of need, and they depend on resilient facilities and flexible, fast response times when the unexpected occurs. In an emergency situation, any delay in responding to the threat will directly impact patient care.
Facilities managers can mitigate a potential loss of services by prioritizing critical improvements and repairs to physical spaces before a disaster hits and having a fast and reliable construction strategy once it does.
Four-step process
As with every discussion about strategy, preparation is key. When it comes to mitigating the impact of a disaster or emergency, there are four key steps:
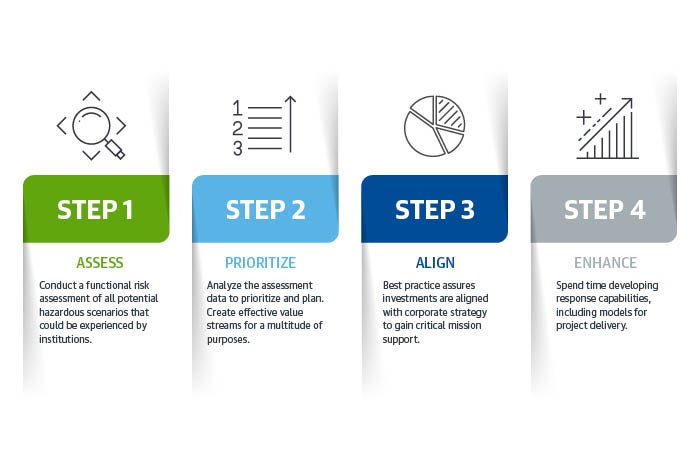
A quick reference tool illustrating the four-step process.
Graphic courtesy of Gordian
Step 1: Gain a better understanding of risks through assessments. Facilities managers know the importance of conducting functional risk assessments of all potential hazardous scenarios that could be experienced by their institutions.
The Centers for Medicare & Medicaid Services (CMS) mandates these risk assessments as a condition of participation; failing to do so can result in suspension or removal of federal funding. However, for a risk assessment to be an effective model to inform investment, health facilities professionals must consider both internal and external challenges.
The identification of external risks associated with patient surge, pandemics, terrorism, loss of utilities, acts of nature and other critical issues should also include analysis and identification of any backlogs of capital renewal or aging infrastructure. Looking at both external and internal threats ensures that stewardship can be properly prioritized for investment.
The challenge for health facilities managers is how to efficiently and authoritatively execute these risk assessments. One specific solution that brings a dedicated and well-defined rigor to this requirement is a hazard vulnerability analysis (HVA). A properly designed and cost-efficient HVA can be a facilities manager’s most powerful ally for helping their organization prepare for potential disruptions and fulfill their CMS compliance obligations for risk assessments.
The most effective HVAs include evaluation of both internal and external risks, which should be analyzed from the perspective of occurrence away from the facility or at the facility. An example would be a terroristic act that sends multiple patients to the emergency department (ED) or a terroristic act directed at the ED. Best practice would also include a facility condition assessment (FCA) to properly define the in-situ condition of the facilities portfolio, ensuring capital renewal and latent infrastructure issues have been properly included in the plan.
The concept of facilities assessment has been around for many years with many constructs from which to choose. The critical goal of an effective assessment is that both capital renewal and deferred maintenance issues are properly evaluated and documented.
As facilities age, they move from their original and designed intent to their current use. In many cases, this negatively effects the risks associated with owning and operating the space and can create significant impacts to mitigate. Patient flow, if not reconciled with the present design and space utilization, can result in serious injury or poor care delivery.
Stewardship funding has often been reduced in back-of-the-house locations, which can lead to significant staff crowding and equipment loading, creating additional operational and safety risks. Utilizing a well-respected standard such as UniFormat® will ensure space is assessed using recognized standards that can be compared to other health care facilities. Comparative analytics is an important concept to align scarce resources to optimize built environments.
Step 2: Analyze the data to prioritize and plan. Once the data has been collected, it can be analyzed to create effective value streams for a multitude of purposes.
Every institution has their own patient care and business priorities, and many integrated delivery networks (IDNs) also have corporate requirements and preferences for capital investment. The health facilities professional will need to ensure the facilities datasets align with those priorities and create a compelling story for the executive team and board of trustees.
One important aspect to remember is that institutions have mission statements that reflect their purpose: patient care, education and research, for instance. A mission statement won’t include “… and facilities” but their mission cannot be achieved without an effective investment plan for capital renewal and deferred maintenance. When the capital renewal and deferred maintenance plan is presented as “critical mission support,” it is more relatable to senior leadership.
The missions advance when the facilities are functioning properly, but when something goes awry, like a power failure, nothing is more important than to resolve the problem quickly and effectively. Ensuring the data sets are in alignment with corporate strategy is paramount to success when coupled with the HVA.
Once documented, the health facilities professional should ensure senior leadership fully understands the elements of the plan and reaches a consensus regarding priorities. Every investment is a complex business decision, and the best plans will include solutions developed within financial realities. Senior leadership cannot reach beyond their financial means to fund a plan that will mitigate all risks. A cash flow strategy that includes multiyear investment models with well-defined needs and priorities is required to address urgent issues while distributing the expense of lower risk elements.
Even the best laid plan will fail if risk mitigation efforts, conditional to sustainment, are not properly planned, prioritized and executed. All risk-based discussions should include both an external and internal scenario.
Step 3: Align facilities investments with critical mission support. Organization of the datasets is paramount to support proper investment. Best practice ensures the investments are aligned with corporate strategy but communicated so the critical mission support message is properly understood by the executive teams.

The critical goal of an effective facilities assessment is that both capital renewal and deferred maintenance issues are properly evaluated and documented.
Image by Getty Images
There are several methods of telling the story to ensure best use of scarce capital. Developing variables that represent corporate strategy and assigning them weights for risk is critical to success. This would include establishing portfolios that align either service line deliveries or space utilization.
For instance, if strategy focus is on orthopedics, then risks to patient flow in the orthopedics service line would be an important criterion. Pinch points in the built environment are places where movement is restricted, leaving patients waiting on hospital beds or rooms to become available in order to receive care. These pinch points can be mitigated, and risk to the orthopedic business can be prioritized from identified vulnerabilities.
Another example of portfolio management might be stratifying acute patient care, non-acute care and support facilities. This method is traditional but can be more effective when the service line issues are addressed between acute and non-acute care patient flow.
Every institution and IDN has its own level of risk aversion. Facilities professionals think of operations in terms of meantime between failures, reliability-centered maintenance or other measurements, and often present their capital needs in that context. Most executives think similarly but focus on care delivery models rather than infrastructure. A helpful metric during the budget cycle to strengthen the correlation between uptime of plant and continuance of clinical care is net asset value (NAV), which is defined as: (replacement value less deferred maintenance) divided by replacement value.
Also known as the percent good remaining in the plant, NAV will help drive consensus regarding current investments and future needs within the portfolio. When coupled with a well-thought-out HVA, the NAV provides a more positive and salient understanding of risk and where the institution is in its facility’s life cycle.
The health facilities professional is now describing what past investments achieved and what investments are necessary to ensure the missions can be properly supported. The facilities professional is no longer competing for capital with the clinical enterprise and has redefined the expense to replace the chiller to ensure mission-critical support for clinical growth. When these needs are put in the context of critical mission support, administration can better understand and relate to the need.
An excellent HVA can become ineffective for many reasons. They include lack of proper analysis and identification, documentation and codification of the issues, consensus on priorities or financial investment shortfalls. The response to potential risks is not always well defined, and traditional project solutions are often unwieldy in times of crisis. Frequently, the HVA receives approval but consensus is not sought or approved for the associated backlogs of capital renewal and deferred maintenance.
To achieve critical mission support, consensus for both the HVA and supporting FCA is required. Risk mitigation is most successful when senior leadership acknowledges that both the HVA and the FCA are the critical paths. Prioritizing mission-critical projects will result in serendipitous outcomes that lower backlogs of deferred maintenance. This might not resolve all the high-priority deferred maintenance needs, but most renewal projects can be linked to infrastructure requirements that support the institution’s overall mission, reducing the backlog.
Step 4: Enhance response capabilities and project delivery methods. The health facilities professional should also spend time developing their response capabilities, including their models for project delivery.
For urgent and recovery projects, the traditional, time-consuming competitive bidding requirements are usually bypassed, accelerating engagement with contractors and other service providers. An expedited response, however, often comes with premium pricing and concerns about quality — unfortunate decisions that impact operations.
It is not enough to have a plan that is aligned with the strategies of the institution. The health care field is embracing new solutions, including value-based construction delivery processes and alternative project delivery methods. High performance includes solutions that support rapid return to normal mission activities and do not create undue hardships on operational budgets.
Strategies for routine project management and service recovery can follow similar paths if planned. Routine solutions generally include flood and water recovery contractors who will respond quickly to mitigate the risks associated with water damage and mold development.
Some general contractors have the bench strength to provide these services, as well. If they are on-site working on other projects, it becomes a simple solution to engage them to bring their resources to bear. When a capable general contractor is not working within the institution, it becomes a much more challenging and expensive activity.
Accelerated projects do not always carry an expedited response price tag. Using an alternative construction procurement method allows facilities to save significant costs and time by bypassing the traditional, time-consuming competitive bidding requirements.
Health care facilities managers can complete large numbers of repairs and renovation projects with a single, competitively awarded contract based on a set of pre-priced construction tasks — an indefinite delivery, indefinite quantity umbrella contracting program known as job order contracting.
This solution is ideal for emergency work and responses to natural disasters because it enables the health facilities professional access to a cache of pre-vetted, professional, qualified and readily available contractors to address the various owner’s project requirements.
Managing the unexpected
Empowering the use of facilities assessments to identify, manage and mitigate vulnerabilities is the first step to successfully managing the unexpected. Data collection is important for prioritizing projects in the wake of an emergency and to facilitate plan true-up after the crisis is mitigated.
Using value-based construction delivery processes and alternative project delivery methods can decrease costs in emergency situations and help to ensure work moves forward with minimal disruption to patient care.
Ultimately, the outcome for the organization is a responsive model that addresses both internal and external vulnerabilities in a timely, transparent and cost-effective process. Most importantly, the negative impact on patients is minimized, allowing institutions to be the heroes the community needs.
COVID-19 has shown that the health care field is very good at identifying local and regional variances in health disparities. The ED has always been the launching point for trauma and critical patient care, and capable of managing most scenarios found in the traditional HVA.
This type of patient surge has resulted in the installation of temporary solutions for patient safety and separation, indoor air quality, triage and patient flow. However, once the national COVID-19 emergency is recalled, these temporary solutions will have to be removed until they’re needed again.
What is needed is a health care facility that is flexible enough to deal with mass influx of critically ill patients that may be presenting with highly transmissible disease. This type of flexibility must include capacities to treat routine patients and maintain elective and emergency surgeries while managing pandemic patients for health facilities to remain viable municipal infrastructure.
Informing the HVA with all critical mission risks will ensure a more resilient and flexible facility that can serve the full community before, during and after crisis. Implementing a job order contracting process will ensure a bench of fully capable and pre-vetted health care contractors to resolve both capital renewal and deferred maintenance backlogs while reducing costs that are associated with disaster recovery.
Mark Kenneday, CHFM, FASHE, CHC, is director of health care market strategy and development for health care at Gordian, a Greenville, S.C.-based provider of facility and construction cost data, software and expertise. He served in various senior health care facilities management positions for more than 35 years and is a past president of the American Society for Health Care Engineering. He can be reached at m.kenneday@gordian.com.




