Planning a system command center

AdventHealth’s command center brings together data and decision-makers to improve the care delivery process for both patients and providers.
Photo courtesy of AdventHealth Mission Control, Orlando
Health systems have been grappling with capacity for years prior to COVID-19, with the pandemic exponentially complicating and exacerbating the issue. AdventHealth’s Central Florida Division – South Region began rethinking the approach to capacity management after it hit a red line in March 2016, when the system could not provide the level of care the community needed due to an unprecedented lack of capacity.
Patients were backed up in emergency departments (EDs) and boarded in hallways, high-acuity transfers could not be accepted, operating rooms were stopped, and elective surgeries were rescheduled. This capacity crisis led the health system to temporarily close its doors to new patients and was cause for an immediate reevaluation of system operations.
AdventHealth’s Central Florida Division – South Region is comprised of nine campuses, with over 3,100 licensed beds and over 22,000 employees. The division functions under a single Medicare license, one electronic medical record system and one medical staff. But, while all campuses are technically under one umbrella, it was not operating as a single system in 2016. Capacity management was siloed, with each facility focusing on its own distinct needs and limitations.
Executive leaders began to explore alternatives that would enable the system to better manage and support patients. While building a new tower was considered, the search for answers went further. After learning about the emergence of health care command centers, the leadership team engaged in a deeper exploration of how a command center could address their needs. That was the beginning of the development of one of the largest health care command centers in the world.
Concept and place
Successful command centers are both a concept, aggregating and analyzing data to create actionable insights, and a place, where key decision-makers whose job functions connect and intersect can be co-located as they collaborate to improve hospital operations. They’re like an air traffic control center for patients.
Well-designed command centers supported by artificial intelligence can help streamline patient flow from dispatch to discharge, improve patient placement processes, decrease inefficiencies, mitigate capacity constraints, and reduce delays in decision-making and care delivery.
At AdventHealth, the command center called “Mission Control” enables the entire division to operate as a single cohesive system. The 12,000-square-foot facility is operated 24/7 and staffed by up to 45 people at one time. The command center’s clinical apps continuously process hundreds of thousands of data elements from more than 10 information systems that flow into the command center every minute.
That synthesized data is displayed as actionable insights, allowing the team to take quick action to resolve and prevent bottlenecks, coordinate patient flow, and make proactive determinations about patient care and staffing needs. These decisions are not just transactional — they’re transformational. Every data point on a screen represents a patient, and with Mission Control as the center of gravity, care quality is elevated across the entire health system.
Steps of development
Developing a successful command center is a multistaged process that includes the following steps:
Creating a vision and aligning goals. For AdventHealth, centralization of resources in a system command center was essential to resolving capacity management issues and achieving the goals of focusing on whole patient care, raising the red line of daily operations, balancing utilization across the system, reducing delays in care and excess days, leveraging existing information technology (IT) investments and providing scalability.
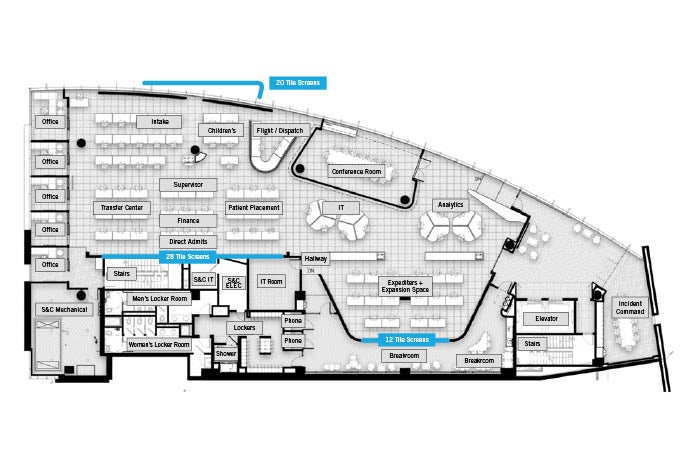
The space layout accommodates both work and respite for 45 staff members working concurrently and includes critical functions such as flight dispatch and incident command.
Floor plan courtesy of HuntonBrady Architects
In seeking a vendor that could quickly help to bring the command center to life, AdventHealth looked at both technology and the change management capabilities. Thorough due diligence led to a partnership with GE Healthcare, which had the technology, experience and resources that AdventHealth required.
Goal alignment began with an in-depth discovery process that brought together over 100 stakeholders across all campuses — from senior leaders to front-line staff. An examination of current processes and challenges revealed that a lack of visibility and gaps in situational awareness were causing inefficient and inequitable use of capacity across the system.
The vision for Mission Control was also informed by touring other command centers and meeting with their leadership teams, including the Disney, NASA, Johns Hopkins and Humber River Hospital facilities. While each center is based on the needs of the organization, seeing scalable operations at a variety of locations provided valuable insights that helped create the right plan for AdventHealth.
Developing the functional design. With the vision established, attention turned to developing the functional design. This five-month process leveraged GE Healthcare’s Digital Twin technology, a collaborative, data-driven methodology used to create comprehensive, integrated improvement plans. By collecting data about existing inpatient and outpatient operations and modeling scenarios that utilized the potential process improvements a command center could deliver, the team gained clarity about how the command center should function to have the most impact.
Testing different scenarios based on growth, bed mix, clinical programs and new efficiencies provided essential insights about which functions, resources and staff members should be centralized within the command center, such as patient placement, transfer coordination, nurse scheduling, admitting, air and ground dispatch, and critical care transporters.
Choosing the location. The next step was to find the right location for the command center. Based on both current needs and projections for the next five years and beyond, AdventHealth had clear specifications about the number of staff and functions that would be collaborating within the space. Proximity to senior leadership and the quaternary center also were important. Structural considerations also were considered, including flood zones, compliance with wind and debris impact resistance codes, and access to a communication backbone.
AdventHealth found the perfect location in some undeveloped space in its executive office tower. While the location was ideal for Mission Control, the space also introduced some design constraints that would need to be accommodated in the final design, including a unique floorplate shape, sound and light issues, existing toilets, a small IT room and large support pillars.
Designing an adaptable layout. With functional design and location decisions made, physical development of the space began. Because the goals and functional design were clearly defined, it took just one year to design and build out the space. The layout included the following critical components:
- Bullpen with pods. This open workspace should be designed to facilitate ad-hoc collaboration and provide easy access to relevant data.
- Offices. A command center requires one or more offices located near the bullpen, usually with glass walls that overlook the central workspace.
- Informal collaboration spaces. The layout includes spaces where both command center staff and visitors can gather.
- Flight dispatch. Special light-emitting diode lighting allows the team to provide a visual indicator to other staff when they are involved in flight coordination, and the design is compliant with Federal Aviation Administration regulations.
- Incident command center. This is integrated into Mission Control to facilitate quick, coordinated responses to disasters such as hurricanes and mass casualty events.
- Respite space. A comfortable, calming space where staff can relax and rejuvenate is essential. It includes spaces that provide staff with privacy to make phone calls or tend to personal business.
- Locker room. Often, staff in the command center will “hot desk” throughout the day, with no specific desk space designated as their own. The lockers provide a space for storage of their personal belongings.
- Raised floor and modular office walls. These elements make new layout configurations quick and cost-effective.
Protecting against fatigue. Command centers are a high-intensity environment, making it important to include design elements that help mitigate operator fatigue. In addition to the break room respite space that’s integral to the command center, AdventHealth’s Mission Control was designed to accommodate staff comfort in the following ways:
- Lighting. Located in sunny Florida within a space with walls of floor-to-ceiling windows, managing natural light and protecting against glares needed special attention. Lighting and shade control systems were installed. In addition, zone lighting ensures maximum control over brightness levels throughout the space during day and night.
- Noise management. Mission Control is located near an urban rail station, and sound studies were done to analyze the acoustic impact. Strategic placement of offices provides a sound buffer, and white noise within the sound system ensures rail traffic does not interrupt critical operations.
- Furniture. Staff members who would be working in Mission Control had the opportunity to provide input about the furniture that would be used in the space, including the option to select their preferred type of desk chair.
Optimizing the technology. Foundational to AdventHealth’s Mission Control operations are Tiles, which are decision support apps within GE’s Command Center platform. The Tiles use artificial intelligence to deliver predictive and prescriptive insights. Highly intuitive, the Tiles provide information that is personalized according to each user’s needs and preferences.
To optimize the use of the large volumes of dynamic information, the design must take into consideration how the data will be displayed and used by the command center team.
For example, video walls, large interactive screens, multiple monitors on desktops, and individual views on phones and tablets are all display capabilities that should be appropriately leveraged based on the specific circumstances. Recognizing whether the data is view-only or interactive will also influence how it is displayed and accessed by the team. Considerations include:
- Where will the data walls be located? How many and which Tiles will be displayed?
- How big should each desk be, and what’s the best monitor configuration on the desks?
- Are there spaces within and outside of the command center that can use large, touchscreen monitors to facilitate huddles, rounding and other regular meetings? Should these monitors be on wheels for easy mobility?
Communication and connectivity to support the command center also need to be considered. For a typical command center, a 1 gigabit per second internet connection is appropriate. In addition, the entire command center facility should be outfitted with generator power to ensure uninterrupted operations.
Providing a showcase. The design of AdventHealth’s Mission Control reflects a commitment to innovation and collaboration. Open ceilings, sound baffles, lighting controls and a tidy appearance all help to deliver a state-of-the-art experience that celebrates technology.
In addition, the space often hosts staff from throughout the system as well as outside visitors and tours. The design accommodates an enhanced guest experience without disruptions to the staff working in Mission Control.
For example, guests arrive in a staging area and can tour the space without interrupting the critical work happening in the bullpen. In addition, a large meeting room in the space is easily accessed near the entrance and has glass walls that can be turned opaque with the flip of a switch.
Put to the test
Mission Control was put to the test just a couple weeks after the opening as a hurricane hit, requiring one of AdventHealth’s facilities to be evacuated.
Historically, coordinating the transfer of evacuated patients to a facility with appropriate capacity would have been a time-intensive process requiring a multitude of phone calls and manual tracking. Instead, with centralized access to capacity management data readily available in Mission Control, the patients were quickly and effectively dispersed throughout the system. Once the hurricane had passed, relocated patients could easily be transferred back to the facility.

The flight dispatch team located in AdventHealth’s “Mission Control.”
Photo courtesy of AdventHealth Mission Control, Orlando
From the beginning, AdventHealth focused on creating Mission Control to better serve patients. While the financial impact was an important outcome, the return on investment was secondary to supporting the needs of the community.
The early results reflect that commitment. Within a few months of deployment, the time from ED admission order to bed assignment had decreased by two-thirds, lateral transfers that helped balance capacity across the system had tripled, and turning away patients because of capacity constraints had been nearly eliminated.
About six months after the command center opened, COVID-19 struck. Now, it is almost impossible to imagine how AdventHealth could have responded effectively without Mission Control, but it is a certainty that outcomes would have been worse.
For early surges, the system used a centralized strategy, bringing all critically ill COVID-19 patients to the quaternary care center. As the surges became faster and larger, the response successfully pivoted to decentralized utilization of critical care resources across the entire system, which provided the ability to preserve critical care capacity for non-COVID-19 patients at the quaternary center.
Precise tracking at Mission Control enabled decisions to continuously balance patient loads, and close monitoring ensured no facility exceeded its capacity.
Time, energy and resources
For health systems considering the deployment of a command center, it is essential to invest the time, energy and resources to develop clarity of vision and goal alignment first. Then, work step-by-step as an integrated team to understand and standardize the processes, define the technology and people to support those processes, and develop the space.
For AdventHealth, beginning with a shared commitment to better serving patients through balanced utilization across the system has led to true transformation. Mission Control supports care progression that is precise and patient-centric with faster turnaround times and fewer delays, where intricate and complex care delivery is simplified for both patients and providers.
Creating a foundation for success
AdventHealth focused on aligning around a single goal — use “Mission Control” to improve systemwide operations with the patient as the central focus. This required a massive cultural transformation for the entire organization based on a collaborative design that grants Mission Control specific decision rights to drive longstanding outcomes. Three key components that underpin this successful transformation are:
- Timely, accurate and actionable data that allows for relational coordination of care.
- An intentionally designed department — space, roles and processes — that provides the ability to synthesize information and caregivers.
- Cultural alignment throughout the organization to activate the change.
Creating this foundation required spending time with the C-suite at each facility to understand their needs and expectations. By gathering feedback from throughout the organization, building a collaborative vision for the command center and standardizing processes across the division, AdventHealth has been able to balance capacity by acting as a single system. The capabilities of the quaternary center are utilized appropriately, smaller hospitals feel supported and the entire community is better served.
A strong facilities management team plays a vital role in facilitating feedback regarding the development of the space and planning resource deployment. In addition to coordinating with outside partners such as the technology provider, architecture firm and construction company, it’s important to engage these internal team members throughout the planning and deployment:
- Medical director of the command center. A respected physician leader who can effectively champion the initiative with the medical staff, ensure alignment and drive change.
- Chief operating officer, chief nursing officer and chief clinical access officer. Determine which senior level executives will serve as the project sponsors.
- Director of patient placement, transfer center, critical care transport and/or patient flow. Find the team members who understand throughput and capacity management across the entire system.
- Central intensivist. The physicians who control intensive care unit access will provide invaluable insights into the optimal command center operations.
- Transfer center leader. The physicians who determine patient placement should be part of the command center development and deployment team.
- Clinical operations leaders, information systems leaders and project managers from throughout the system. Seek team members who understand daily operations at the local level and can help standardize and centralize workflows.
Sanjay Pattani, M.D., MHSA, FACEP, is the associate chief medical officer at AdventHealth Orlando; Penny Porteous, MSA, BSN, R.N., is executive director of Mission Control at AdventHealth Orlando; and Ryan Treml is managing director at GE Healthcare Partners. They can be contacted at sanjay.pattani.md@adventhealth.com, penny.porteous@adventhealth.com and ryan.treml@ge.com. Contributing authors are Greg Braithwaite, AIA, ACHA, vice president/healthcare principal at HuntonBrady Architects, and Jeff Terry, FACHE, founder and CEO of GE Healthcare Command Centers.




