Equipment planning for imaging suites

Computed tomography machines are the workhorses of health care facilities, which is why they’re seen in every emergency department and inpatient hospital.
Image by Getty Images
Regular health care construction projects are instrumental in keeping the lights on in the incredibly demanding health care field. More specifically, the state of facilities is critical to patients’ perceptions of care quality; employee attraction and retention; and compliance with ever-evolving facility standards, environmental requirements and building codes.
Therefore, a health care construction project goes way beyond slapping a new coat of paint on the walls. Often, it requires years of active construction. And, although there will always be hurdles to any project regardless of industry or building type, health care construction projects are uniquely difficult to navigate — whether dealing with lengthened equipment lead times or additional budget considerations.
However, evolving technology’s impact on equipment planning in hospitals poses an especially interesting challenge. As equipment technology progresses, so does the desire to have it all integrated and connected to the facility’s electronic health records, or just as simple as a connection to the internet for manufacturer access and supervision.
This creates the challenge of trying to anticipate not only the connections to the network but also the protection of the network or providing multiple hard-wired or wireless networks and, more importantly, the infrastructure and space for conduits cabling and wiring.
Among these challenges is ensuring medical equipment planning is integral with the design and construction for the high-acuity areas of imaging and hybrid rooms.
Equipment evolution
Although the mechanical portions and units of diagnostic modalities have become more physically compact, they now require a lot more infrastructure support and planning — specifically regarding data transfer and storage. To illustrate, consider computed tomography (CT) machines.
This piece of medical equipment is the workhorse of health care facilities, which is why it’s seen in every emergency department and inpatient hospital. The core units themselves haven’t changed much beyond efficiency updates to produce higher-resolution images and lower the radiation footprints. At face value, these machinery updates don’t seem to affect facilities too much. However, as pieces of medical equipment grow more sophisticated, people begin to use them differently.
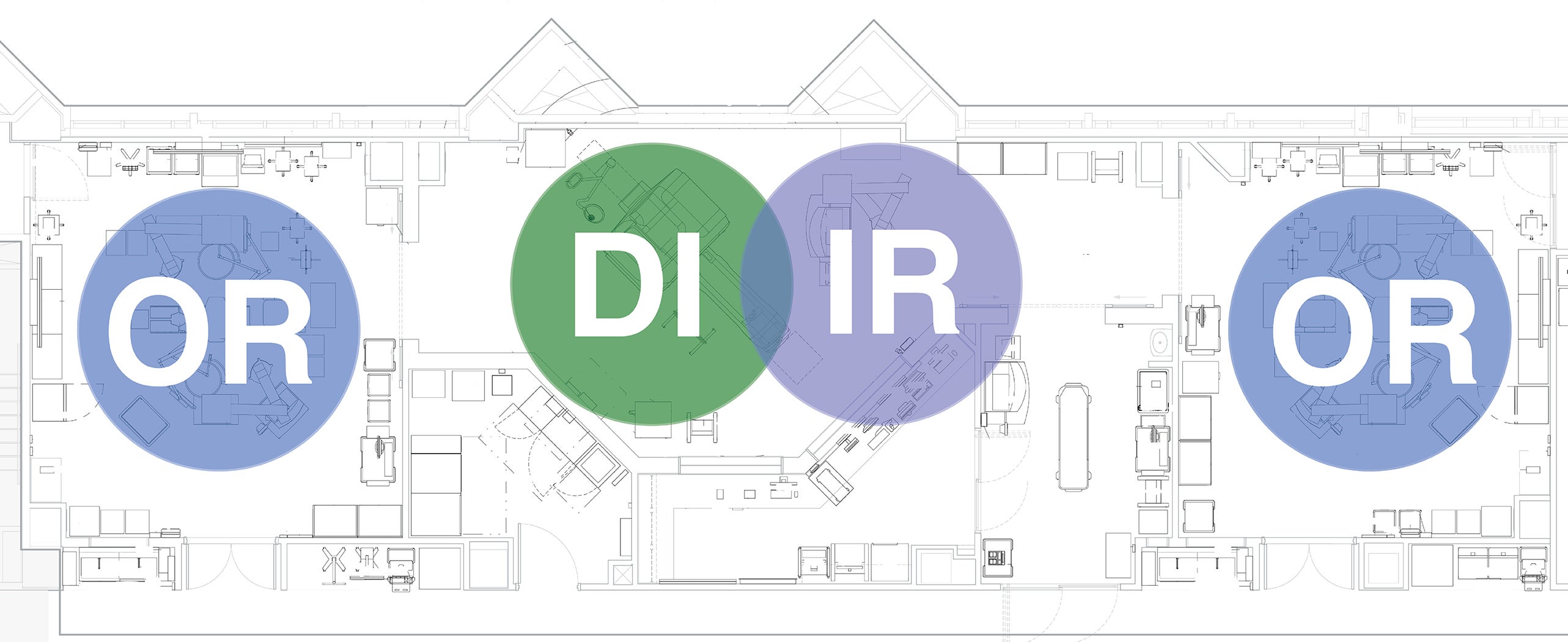
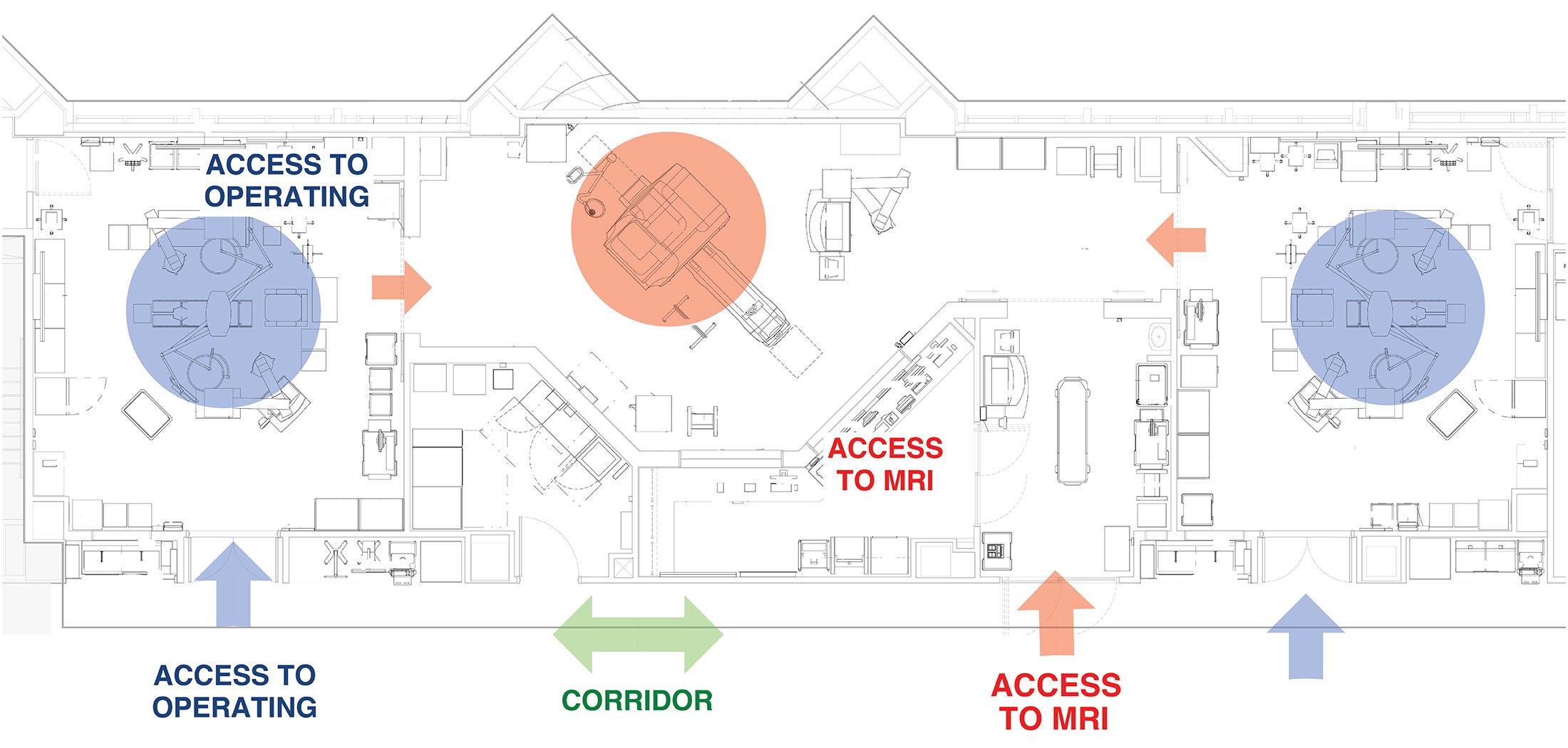
For instance, more hospitals are incorporating intraoperative magnetic resonance imaging (iMRI) suites in their facilities. These suites, which sit adjacent to operating rooms (ORs) and allow surgeons to obtain imaging in the middle of surgery (among other modalities), were basically unheard of 10 years ago. It is now common practice for hospitals to add robotic systems into their new operating suites to stay competitive. Today, it’s rare to do any health care construction project that doesn’t include a hybrid OR with at least infrastructure for robotics.
Project management teams must be sure to consider who will use the medical equipment and how it’ll be implemented. This will reduce internal conflicts and ensure smooth workflows. MRIs have typically been part of the diagnostic imaging (DI) departments, but when imaging and surgery merge in this suite setting, surgeons and diagnostic specialists must work in symbiosis.
This type of suite creates the opportunity to add interventional radiologists (IRs), who perform minimally invasive surgical procedures while patients are in MRI machines, as part of the iMRI suite. As medicine advances and technology evolves, IRs have introduced additional procedures, requiring more medical equipment inside the suite. So not only does a project management team have to plan for additional medical equipment in the room, but it also must ensure that the equipment integrates with the imaging and hospital system, meets MRI and surgery requirements, and is adaptable enough to future-proof construction.
Future-proofing sounds straightforward enough. And in some ways, it is. For instance, it’s good practice to install extra conduits to account for future use cases. However, full-scale future-proof construction is much more complicated, especially when considering how much time it takes to get medical equipment planned, ordered, delivered and incorporated into workflows during active renovations.
For instance, MRI machines have about a 40-week delivery timeline from order to delivery. Before ordering, project management teams have to think about how they’ll get it in (and eventually out) of the building. Once it arrives, they must account for a two-month installation and commissioning period. Basically, they are looking at a year from order to first use, not including planning and design time.
Making a room bigger or outfitting the walls with removable panels is one thing; getting the unit to an upper floor of the hospital is another entirely. Project management teams can’t simply load it onto an elevator. At its lightest, an MRI machine weighs about 16,000 pounds. Instead, they need to prepare an equipment installation plan in advance, which will likely involve cutting a hole on the side of the building so a crane can move the unit in.
Moreover, it’s not uncommon for health care construction projects to span more than four years. As a result, project management teams must make physical room for additional medical equipment installation and consider the future of health care technology. Building codes and regulations will undoubtedly change in that time too, and teams need to be ready to adapt to them.
Texas regulators, for instance, once deferred to manufacturers on the size of the imaging rooms. More recently, however, they have started requiring 4 feet of passage space around the units. As a result, architects who work on Texas projects have had to increase the size of the rooms to ensure they’re up to code. These situations are precisely why future-proofing construction can be so difficult.
Better equipment planning
Fortunately, hospital decision-makers can employ future-proofing strategies to prioritize innovation while improving connectivity and standards across the health care system. These strategies can be broken down into project management and construction categories.
Project management strategies. When it comes to health care construction projects, there are a lot of moving parts. That’s why it’s important to start planning early. Tips to help facilities professionals better prepare include:
- Give the right information at the right time. There’s generally a 20- to 40-week lead time on major medical equipment, and technology can evolve over that time. So, contracts will often be outfitted with clauses specifying that the manufacturers must deliver the latest technology at the time of installation for no upcharge. That means if a project team orders a Model 10 today and a Model 11 is released two months before installation, the manufacturer is obligated to deliver the Model 11.
This change has a trickle-down effect on medical equipment installation contractors, which is why timing and communication are crucial. If the project management team must adapt its plans to fit a new model, it will ultimately be charged for the redesign work. Alternatively, the team can hold a design fee, contractor fee or allowance for the specific room. The engineer and architect will wait to design the room until the equipment is ready, but that could be more than two years away. Either way, the project management team must pay — it’s just a matter of when.
A recent facility project involved renovating two existing floors that included ORs, hybrid rooms and a CT scanning room. After meeting with all parties, the designers decided to phase the work. They previously worked on a similar project and had to go through costly redesigns time and again due to changes in technology and operational requirements as well as the construction times associated with renovating two full floors at once. The project was not only built and equipped in phases but also planned and procured in the same fashion to reduce the costs of changes and technology obsolescence.
- Get estimates early. Estimates and budgets are two different things in the world of planning, design and construction. Medical equipment planning provides estimates on equipment costs for one straightforward reason: Equipment planners can’t control medical equipment prices. Instead, they build a report that includes estimates for all the equipment and contingencies when planning a facility for a health care system. They use real-time prices instead of list prices for their estimates based on their current purchase averages. So, it’s best to involve an equipment planner as early as possible when setting goals for equipment spending strategies.
The later the equipment teams get involved in the planning and design process, the harder it will be to align the equipment needs with the facility budget. This is especially true if it was set without incorporating the associated equipment and supplemental costs. At this point, the conversation turns to reduction strategies. These strategies usually involve deferring purchases, finding alternative funding methods or, in a worst-case scenario, reducing the functionality or quality of the equipment below the original expectation to meet a budget.
- Lay out the decision path. The past two years have been erratic when it comes to medical projects and equipment. Medical supply chains bore the brunt of fluctuating supply and demand, pushing medical equipment delivery timelines far back. Pharmacy hoods, for example, went from eight weeks to nine weeks to 12 months. When the COVID-19 vaccines rolled out, a refrigerator couldn’t be purchased anywhere. Consulting and engineering teams had to constantly communicate with manufacturers and distributors to properly advise health care organizations on these changing time frames. That way, the purchasing decisions could be made in time to align with the project schedules.
Therefore, it’s imperative to develop a schedule with the equipment planner that includes purchasing time frames and a go-live date. If a project management team wants to go live on an exact date, it will need a certain number of days for planning, purchasing, production, delivery and installation. So, the team needs to start making decisions on what it wants to buy. In some cases, the team can stretch the timeline of these decisions. Generally, it’s best to begin the purchasing meetings 18 months ahead of a hospital’s go-live date. Sometimes, this includes selecting and buying equipment before the design is complete.
Construction strategies. Once construction begins, it becomes a lot harder to pivot. The following strategies can help ensure the process goes smoothly:
- Choose the right room size and technology. In some ways, choosing the right room size is cut and dried: Manufacturers must meet Occupational Safety and Health Administration requirements — and the project management team must follow these specifications, too. However, if one looks at a manufacturer’s drawings for an MRI machine, they’ll see that they don’t consider anything else in the room other than the one machine. Realistically, that room needs to be outfitted with supply closets, physiological monitors, injectors, linen hampers and other pieces of equipment. Therefore, the team needs to decide how much to increase the square footage to account for additional technology and medical equipment.
For instance, patients will likely be wheeled into the room on bulky stretchers in an inpatient setting. And, in the case of a hybrid OR, they might even be on general anesthesia. In that case, the project management team will need to build more space for the anesthesia machine, which is about 12.5 square feet. Failing to account for other medical or non-medical equipment is one of the biggest holes in medical equipment planning, so teams must be careful not to fall into the trap.
- Maintain flexibility for manufacturers’ models. Equipment changes about every three to seven years. During that time, medical equipment manufacturers race to release leading-edge models. Once one manufacturer releases the blueprint, the rest scramble to copy the design and get it out to market. Maintaining flexibility in planning helps a facility absorb some of these changes with minimum impact.
Plus, in DI equipment, the changes are typically software related. That’s by design. Manufacturers know that existing hospitals don’t have the extra square footage to install larger medical equipment, so manufacturers try to keep their updates restricted to the existing footprint.
- Ensure infrastructure support for technology. Hindsight is 20/20, but that hindsight comes with a price tag in health care construction. Of course, project management teams are never able to foresee every future need, but they can take a few steps to ensure infrastructure support for future technology.
For instance, imagine a facility has an MRI machine that is just running basic scans for the time being. If the facility has any plans for IRs to do procedures in that MRI machine in the future, however, it will need a wall-mounted monitor where the IRs can view images. Adding blocking in the infrastructure so that the monitor can someday share images is exceptionally cheap (approximately $500) if it is installed while the room is being built. On the other hand, installing such infrastructure after the fact will cost tens of thousands of dollars and take much longer to complete.
- Follow future-proof planning. The pace of technological advancement is so great in the health care field that it’s not a good idea to plan for construction more than five years in advance. If a project management team wants a 10-year plan, it’s better to masterplan and allow for flexibility rather than focus on details of current equipment.
Staying up to date
It’s not easy to keep a health care facility up to date and future ready. But it’s not impossible, either. Health facilities professionals must find a good project partner who can help them keep an eye on the future of health care technology and watch as their health care organizations lead the way.
Florida hospital expands technology to handle growing patient population
A few years ago, the University of Florida Health Shands Hospital realized referral patient demand at its main campus in Gainesville, Fla., was quickly exceeding capacity.
The health system knew it needed to expand its facilities to better serve a rising patient population, improve access to care and ensure a positive patient experience. As part of its continued future-proofing strategy, UF Health Shands green-lit the construction of a specialty tower that would neighbor its cancer center and provide state-of-the-art care to patients with neurosurgical, neurological and cardiovascular conditions.
UF Health Shands needed a technology consulting and engineering firm to design and construct several prominent towers on its main campus. The system’s leadership team tapped Introba to lead visioning services to marshal these specialties around familiar technologies. It leveraged the interventional suite’s programmatic and spatial arrangement to satisfy the diverse needs of these distinctive specialties.
In the end, the project spanned approximately 500,000 square feet. Construction costs sat a around $400 million, including an equipment budget of nearly $100 million. Almost 18 operating rooms (ORs) were designed within an integrated platform to leverage common core support elements, such as central supply and anesthesia support for hybrid neurological and cardiovascular ORs, and trauma and general ORs.
The new specialty tower, completed in 2017, contains 216 beds, including acute care and intensive care unit beds. It also has clinics and diagnostic areas for neurological and cardiovascular assessment, prep and recovery, pharmacy and pathology.
About this article
This article is based on a presentation given by the authors during the 2022 International Summit & Exhibition on Health Facility Planning, Design & Construction.
Pier Vettorazzi, AIA, IIDA, LEED AP, is director of planning and project management for medical equipment planning, and Lisa Charrin, AIA, ACHA, is vice president of medical equipment planning at Introba. They can be reached at pier.vettorazzi@introba.com and lisa.charrin@introba.com.