Changes to health care ventilation requirements

Outpatient facilities, like this Southern Ohio Medical Center medical office building in Vanceburg, Ky.,will be impacted by the 2024 ventilation standards and guidelines in ANSI/ASHRAE/ASHE Standard 170.
Photo © 2023 Lauren K Davis, Feinknopf
First published in 2008, the American National Standards Institute (ANSI)/ASHRAE/American Society for Health Care Engineering (ASHE) Standard 170, Ventilation of Health Care Facilities, has profoundly impacted health care facilities across the country over its brief 15-year history.
Standard 170 was included in the Facility Guidelines Institute’s (FGI’s) 2010 Guidelines for Design and Construction of Health Care Facilities as well as the subsequent versions of the Guidelines. Adoption of Standard 170 continued with the 2012 edition of the National Fire Protection Association’s NFPA 99, Health Care Facilities Code, and the 2015 edition of the International Code Council’s International Mechanical Code.
With enforcement of the standard by The Joint Commission, Centers for Medicare & Medicaid Services and local code authorities, the quick adoption of Standard 170 by multiple organizations means the standard has become an essential document for health care facilities managers and designers.
Continuous improvement
ASHRAE has a robust process for updating its standards called “continuous maintenance.” ASHRAE brings together multiple volunteer stakeholders comprised of owners, designers, producers, contractors, authorities having jurisdiction and, in the case of ANSI/ASHRAE/ASHE Standard 170, infection prevention practitioners to form a Standing Standards Project Committee.
The full committee currently has 67 members comprised of full committee voting members, subcommittee voting members and consultants, with 17 full committee voting members making the final determination on changes.
Once the full committee has decided to change, delete or add language to the standard, it is released for public review as a proposed addendum on ASHRAE’s website for either a 30- or 45-day public review period, based on the quantity of the changes proposed.
While the addendum is out for public review, anyone may provide comments to the committee about the proposed changes, which it can then consider before final publication. The committee must respond to all comments submitted during the public review period.
Once all comments have been addressed by the committee and all required public reviews are complete, the addendum is published and placed on ASHRAE’s addenda website for users of the standard. The standard is published every four years to correlate with the FGI Guidelines. Each publication is based on its previous iteration, plus all addenda that had been published since the previous publication.
The 2021 edition
Incorporating 17 addenda, the 2021 publication of ANSI/ASHRAE/ASHE Standard 170 was released in the first half of 2021. Its users will notice changes in the document from start to finish. The title, purpose and scope of the standard were changed in addenda q because the temperature and humidity requirements of the standard are not comprehensive thermal comfort requirements for each space (comfort is more comprehensively covered in ASHRAE Standard 55).

The penthouse at Southern Ohio Medical Center’s outpatient facility locates all HVAC systems indoors, keeping equipment sheltered from the elements to improve resiliency and ease of maintenance.
Photo courtesy of Heapy
Several addenda to Section 3 included adding definitions for inpatients, outpatients, residents and Class 1, 2 and 3 imaging spaces, as well as updated definitions for invasive procedures, operating rooms and procedure rooms.
Addendum e modified parts of sections 5 and 10 to bring all the planning elements into Section 5 and allow Section 10 to provide requirements for construction and system start-up, with some new requirements for construction and system start-up added to the standard.
Section 6, Systems and Equipment, was modified by addenda a, d, i and p to address filters, outdoor air intakes, additional ventilation standards and humidification requirements.
The first change that users of the standard will notice is from addenda d with the addition of Table 6-1, which addresses minimum separation distance from relief/exhaust locations and outdoor air intake locations. This helps add clarity to separation distance to trash locations as well as discharge locations for Class 2 air, which may be odorous from a space like a dining area but doesn’t represent a concern of contaminants.
Another change is the removal of Table 6.4 addressing required filtration levels. The presentation of minimum filtration requirements in Table 6.4 allowed for different interpretations and understandings of minimum filtration requirements and led to inconsistent application of the standard.
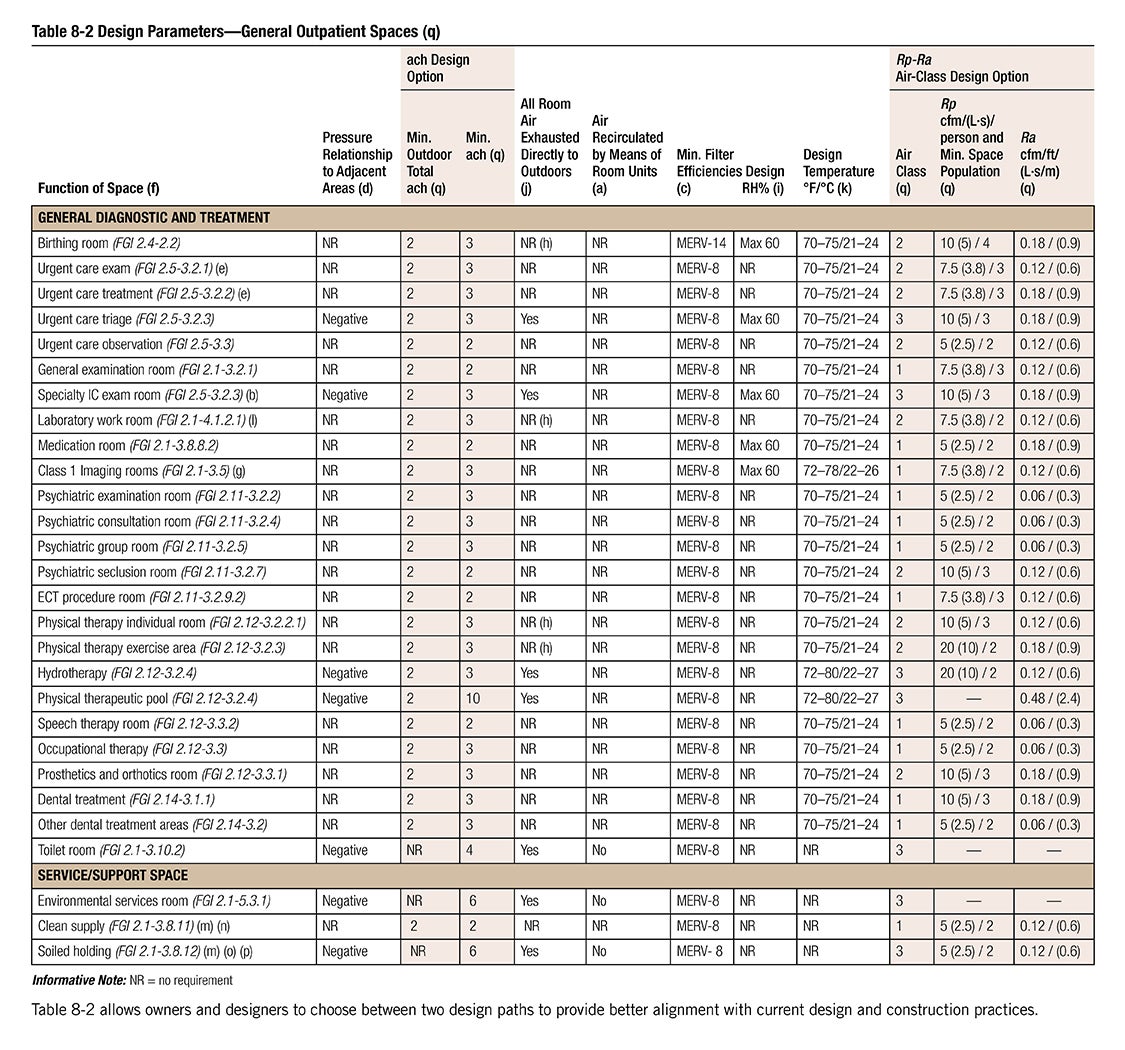
The standard now shows all minimum filtration requirements embedded in tables 7-1, 8-1, 8-2 and 9-1 at the function of space level, removing the ambiguity of the requirements from Table 6.4. These changes were incorporated into addenda a and p. Addenda i added requirements to the standard addressing adiabatic high-pressure humidifiers and maintaining water at a temperature within the control limits of the facility legionellosis risk management plan.
Sections 7, 8 and 9 saw the most significant revisions as the standard continued alignment with the 2018 edition of the FGI Guidelines. Section 7, Inpatient Spaces, was improved in addenda a and p by adding an “Unoccupied Turndown” column and “Minimum Filter Efficiencies” column to Table 7-1.
The “Unoccupied Turndown” column helped clarify which spaces could be designed to reduce airflow below the minimum total air changes per hour while the space is unoccupied, allowing for reductions in energy needed for cooling, fans and reheat. Addendum m added behavioral health spaces to the table, including patient bedrooms, resident rooms and seclusion rooms.
This provided clear direction to designers on proper pressure relationships, outdoor air changes per hour, total air changes per hour and minimum filter efficiency requirements. The filter requirements for operating rooms, caesarean delivery rooms and Class 3 imaging rooms were increased from MERV 14 to MERV 16, with operating rooms or Class 3 imaging rooms designated for orthopedic procedures, transplants, neurosurgery or dedicated burn unit procedures now requiring HEPA filters be provided at the air terminal device.
The last addendum incorporated into the 2021 edition of the standard (addendum s) took lessons learned from the COVID-19 pandemic and provided a path for airborne infection isolation (AII) room exhaust to be combined with general exhaust as long as it passes through a HEPA filter first. This change provides flexibility for owners to choose how they want to handle AII room exhaust in new buildings and greater certainty of the authority having jurisdiction accepting the approach for existing facilities.
While Section 8, Outpatient Facilities, included the addition of minimum filter efficiency concepts discussed previously for inpatient facilities, the committee addressed differences in minimum design requirements based on outpatient acuity by creating a Section 8.1 for Specialized Outpatient Facility requirements and Section 8.2 for General Outpatient Facility requirements.
The specialized outpatient facilities include outpatient surgical, endoscopy, infusion, renal dialysis, freestanding emergency departments and imaging facilities with Class 2 and 3 imaging rooms, which aligns with FGI facility types, and the requirements for the spaces in these outpatient facilities are consistent with similar spaces in inpatient facilities.
The general outpatient facility requirements in Section 8.2 are intended for those outpatient facilities not included in specialized outpatient facilities that will tend to see lower acuity patients. Many of these facilities are traditional doctors’ offices found in medical office buildings. Historically, many of these facilities were not designed to meet the air change per hour requirements included in Standard 170, instead using more typical office ventilation rates.
Table 8-2 (see next page) allows owners and designers to choose between two design paths: utilize the more familiar health care design approach of air changes per hour but at lower rates due to lower acuity patients, or employ an approach based on outdoor air ventilation rates determined by the area of the space and maximum number of persons expected in the space, matching the approach of ANSI/ASHRAE Standard 62.1. These changes are anticipated to provide better alignment with current design and construction practices for these facilities.
Section 9, Residential Health, Care, and Support Spaces, saw improvements by revamping Table 9-1 to include space types for hospice facilities and assisted living facilities in addition to the already included nursing homes, service and support spaces. Table 9-1 saw similar clarity improvements with an “Unoccupied Turndown” column and minimum filter efficiency requirement added to the table. Designers and owners of “Residential Health, Care, and Support” facilities should find the updated standard to be a significant improvement.
Coming in 2025
There are currently seven addenda to the 2021 standard that are published and available to the public. Addendum e added to the standard requirements on how to implement natural ventilation in a health care setting; early versions of the FGI Guidelines stated that natural ventilation was permitted, but it wasn’t clear to users how this would comply with Standard 170.
The addendum permits fan-assisted natural ventilation to ensure that room air changes are being met and specifically exempts the naturally ventilated outdoor air from having to meet the filtration requirements of the standard.

Caption goes hereSouthern Ohio Medical Center’s outpatient facility houses a family practice for four doctors with 12 exam rooms, as well as rehabilitation areas, a retail pharmacy, a lab draw area and an imaging department.
Photo © 2023 Lauren K Davis, Feinknopf
While natural ventilation in all climates won’t make practical sense, it allows flexibility and potential energy savings for those clients that can benefit from natural ventilation.
Addenda d and g continue alignment with FGI definitions for Class 1, 2 and 3 imaging rooms as well as provide a definition for hybrid operating rooms. Addendum g also provides an update to Table 6-2, Supply Air Outlets, requirements for operating rooms, procedure rooms and Class 2 and 3 imaging rooms.
Earlier versions of this table lumped operating rooms and procedure rooms in the same line of the table, which gave the appearance that procedure rooms could require group E, nonaspirating supply diffusers, but this was not the intent because procedure rooms do not have primary supply diffuser arrays.
Addendum g made clear that operating rooms and Class 3 imaging rooms have the same diffuser requirements that operating rooms traditionally have, and that procedure rooms and Class 2 imaging rooms only require group E diffusers. Addendum g also clarifies requirements for when nuclear medicine requires exhaust and negative pressure.
Addendum f revises how ANSI/ASHRAE/ASHE Standard 170 ventilation calculations are integrated with ASHRAE Standard 62.1 ventilation rates. Prior to the addenda, Standard 170 ventilation rates were integrated into the multiple zone formula contained in ASHRAE Standard 62.1. Now, spaces covered under ASHRAE Standard 62.1 are calculated per that standard, and spaces under Standard 170 are summed and added to the calculation from ASHRAE Standard 62.1.
Addendum h continued the process started in the 2021 version of defining unoccupied turndown requirements for specialized outpatient facilities while addendum j continued adding to the behavioral health space by defining ventilation rates for group settings.
There are several addenda undergoing the public review process (i.e., addenda i, k and L), with public review occurring this fall. Addenda i clarifies many different complex situations that can arise when an exhaust stack discharge is required for airborne infection isolation rooms, bronchoscopy and sputum collection exhaust, pharmacy hazardous-drug exhausted enclosures and laboratory work area chemical fume hoods.
The addendum makes clear that the minimum 10-foot discharge is based on height above the service access level (to protect maintenance personnel) and that it must be higher than any roof surface within 4 feet (accounting for situations with different roof levels or sloped roofs), at least 6 feet from exterior walls and at least 30 feet from outdoor air intakes, openable windows or doors and areas that are normally accessible to the public.

The hot water heating system at Southern Ohio Medical Center’s outpatient facility provides energy efficiency with condensing boilers and supply water temperatures below 140 degrees and resiliency by eliminating single points of failure and redundant equipment.
Photo courtesy of Heapy
Proposed changes in addendum k address the reserve design capacity requirements of the standard contained in Section 6.1.2. The proposed changes now treat central heating and cooling systems the same, requiring that central heating and cooling sources for operating, delivery, birthing, labor, recovery, emergency, intensive care, nursery, resident care areas and inpatient/resident rooms have reserve design capacity for when equipment is not operating due to breakdown or routine maintenance.
The standard now also indicates to owners and designers that water storage should be evaluated for steam for building heating and domestic hot water production.
Proposed changes in addendum L address a reorganization of Section 10 with an improvement on the language for use of HVAC systems during construction. Some of the changes include applying filter media over outdoor air intakes when outdoor dust-generating construction activities are occurring within 35 feet and maintaining negative differential air pressure in indoor construction zones relative to occupied areas. Other changes under committee consideration likely to be included in the 2025 version are improved clarity on room recirculation units. This would provide a clearer definition of what a room recirculation unit is, create subcategories of room recirculation types and indicate the subcategory that may be used in each space.
Lastly, the committee is looking at the emergency conditions document that FGI published in early 2021, which addressed pandemic and other emergency conditions, as well as appropriate ventilation items to bring into Standard 170 as a minimum requirement.
The proposed changes to Standard 170 are likely to be released for public review late this year and in early 2024, especially if they are to be part of the 2025 standard.
Evolving and adjusting
After a busy 15 years, the committee responsible for the ANSI/ASHRAE/ASHE Standard 170 continues to evolve and adjust to the changing needs of the health care facility environment.
ASHRAE/American Society for Health Care Engineering (ASHE) Guideline 43, Operations Guideline for Ventilation of Health Care Facilities, is a proposed guide document under development for several years by ASHRAE and ASHE to assist health care facilities managers with the operation of the ventilation systems within their facilities.
With the publication of the American National Standards Institute (ANSI)/ASHRAE/ASHE Standard 170 in 2008, the design requirements within the standard have occasionally been misunderstood. Guideline 43 addresses operational aspects to allow for more consistent application of surveys by state agencies, the Centers for Medicare & Medicaid Services and other accrediting agencies by filling the gap between design requirements and operational practice.
It provides operational guidelines for implementing maintenance programs, monitoring spaces and operating practices in addition to recommendations for inspection and maintenance tasks. It addresses legacy systems by evaluating them against the standard for which they were designed, or for those systems without an established design standard, evaluating against ANSI/ASHRAE/ASHE Standard 170‑2008. The guideline directs users to develop a maintenance program that preserves the capability of the HVAC systems to provide thermal comfort, energy efficiency and indoor air quality. Other important inclusions of the guideline include relative humidity excursions and temperature variances.
Monitoring spaces addresses the criticality of the space with regard to patient risk and, based on that criticality, recommends the frequency of validating room pressure, temperature, humidity and airflow. Operating practices provides a framework for helping facilities managers with the day-to-day balance of immediate short-term issues, scheduled needs, ongoing building rehabilitation and construction projects, and long-term visioning and capital planning.
The recommended inspection and maintenance tasks section provides guidance for air and water distribution systems, air-handler equipment, boilers, chillers, coils and radiators, control systems, heat rejection equipment, dehumidifiers, humidifiers and others. Each equipment type includes a table of recommended inspection and maintenance tasks along with frequency and corrective action for these tasks.
The first public review of Guideline 43 began in late 2023 and, depending on the quantity and types of comments, could be published within the next couple of years.
Jeremy Fauber, PE, CGD, LEED AP BD+C, is principal and engineering manager at Heapy and committee chair of ANSI/ASHRAE/ASHE Standard 170, Ventilation of Health Care Facilities. He can be reached at jpfauber@heapy.com.