2011 Hospital Energy Management Survey
About this survey report
Health Facilities Management (HFM) and the American Society for Healthcare Engineering of the American Hospital Association surveyed a random sample of 4,865 hospital executives to learn about trends in hospital energy management. The response rate was 14 percent, or 691 completed surveys.
HFM thanks the sponsors of this survey — Amerinet, Gardner Denver, Schneider Electric and Skanska USA Building.
|
| Click here or the above image for a PDF of the survey. |
Two years removed from the Great Recession, hospitals and health systems are putting the oomph back into energy-efficiency efforts.
The hold-downs that squeezed facilities budgets are easing and organizations are devoting more attention and resources to energy-conservation initiatives,
That's welcome news for hospital facilities managers who have tried to do more with less during this economic crisis. Renovation is picking up, more money is becoming available for projects and there's a sense of renewed optimism about the level of activity, says Dale Woodin, CHFM, FASHE, executive director of the American Society for Healthcare Engineering (ASHE).
"It's not back to where it was three or four years ago," Woodin says, "but people are realizing we're coming out of this thing and it's time to get back to business."
Progress and shortcomings
A review this spring of energy management initiatives under way around the country found signs of progress as those efforts regain momentum, but also testified to the many shortcomings and missed opportunities.
While awareness of various energy-saving options is up, the 2011 Hospital Energy Management Survey conducted by Health Facilities Management (HFM) and ASHE showed that a majority of organizations still are not taking such basic recommended steps as performing regular energy audits, creating a strategic master energy plan, using commissioning of existing buildings or following the Green Guide for Health Care to monitor baseline energy performance. Those that do conduct audits frequently fail to follow up to make sure that deficiencies are fixed.
On the positive side, large percentages of respondents cited plans to implement those or other initiatives in the next 24 months and most already have pursued what Woodin calls the low-hanging fruit of energy conservation measures, such as preventive maintenance and more energy-efficient lighting.
The percentage of those who say they participate in the Environmental Protection Agency's (EPA's) Energy Star program has doubled since HFM/ASHE conducted the last survey five years ago. And the percentage of facilities to have upgraded central heating and cooling systems in the past two years (40 percent) has risen sharply from the 2006 survey.
Numerous responses to the survey suggest that funding for initiatives remains tight in many places. But a lack of resources shouldn't stop facility managers from finding ways to boost energy efficiency and savings, says Delbert Reed, CHFM, SASHE, director of facilities engineering at Ben Taub General Hospital in Houston.
"There's a tremendous amount of savings that can be achieved beyond what we're saving now," says Reed, who's on an energy-management task force at ASHE that's compiling energy-management strategies to share with members. "You don't understand how many millions of dollars' worth of opportunities you're walking past every day. People think, 'Oh, that's not going to save me very much.' But it can be something as simple as turning off a light."
Ben Taub saved more than $800,000 a year in avoided energy costs, he says, by reducing the pressure level on its boilers to 65 psi from 110, ending the practice of always keeping a backup boiler idling, and adjusting air and water temperature settings to the original design specifications. Energy costs per square foot dropped from $4.61 in 2008 to $3.85 in 2010.
Moreover, many energy-saving operations built into facility designs are overlooked or not being taken full advantage of, according to Jamie Qualk, vice president and team leader of the sustainable solutions group at Nashville, Tenn.-based SSRCx, a division of the Smith Seckman Reid consulting firm. In the thermal distribution system, for example, oversights such as dampers that aren't linked or operating properly and valves that weren't installed correctly or don't open or close right can have a huge impact on energy consumption when added together, he says.
Overall, however, industry-watchers say facility managers and energy-related efforts in general are moving in the right direction. "While we still have many more things we can do, we're on the right track," Qualk says.
Major trends
Other issues raised by respondents to the HFM/ASHE Hospital Energy Management Survey include the following:
Aging energy hogs. A wide diversity of facility types was represented among the 691 organizations responding to the HFM/ASHE survey, which was conducted online in March and April by Perception Solutions Inc., Aurora, Ill.
Acute care hospitals almost certainly are the biggest energy users among them, resulting in health care ranking second behind the food-service industry in total energy consumed per square foot among commercial buildings, according to the Department of Energy. It doesn't help the energy conservation cause that despite the building boom of the past decade, most main hospital buildings — including those of 69 percent of the survey respondents — still are more than 20 years old. The performance of energy-consuming systems degrades by as much as 30 percent in the first few years of operation, according to the American Society of Heating, Refrigerating and Air-Conditioning Engineers.
Yet age isn't always the best indicator of energy performance, since older buildings can benefit from equipment upgrades and renovations. For example, a 191-year-old bank in Cambridge, Mass., is Energy Star-certified, notes Clark Reed, director of the health care facilities division for the Energy Star program.
Insufficient audits. There's no consensus on how often or thoroughly to conduct energy audits, which can range from simple walk-throughs aimed at identifying low- or no-cost measures to more sophisticated, expensive reviews. About 28 percent of poll respondents said they perform an energy audit in their acute care hospital at least annually, while another 25 percent said they do theirs every two to three years — results that were little-changed from the 2006 survey.
Experts say the exact time between audits isn't as important as doing them regularly and following up on the recommendations.
Facility managers need to take charge until they can rely on fully automated systems that will control temperature, humidity and air-flow levels precisely, plus engage emergency generators to prevent failure of electrical grids, according to Dan Chisholm Sr., emergency power system expert for MGI Consulting Inc., Winter Park, Fla.
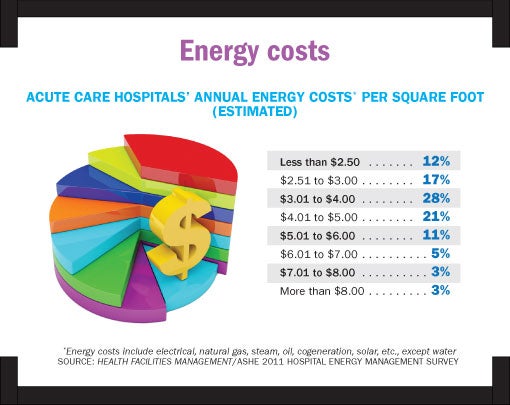
Stable costs. Energy costs have not changed dramatically in five years. More poll respondents (29 percent) cited annual costs of $3.01 to $4 per square foot at their acute care hospital than any other price range, the same as in the 2006 survey.
Just as five years ago, however, more than 40 percent paid more than that, with climate and location obviously key factors (hospitals in Alaska, Florida, California, the arid Southwest and the Gulf Coast tended to report the highest costs).
About 43 percent of surveyed organizations saw annual energy costs rise from the previous year, with the most common response (30 percent) being an increase of between 1 and 5 percent. But nearly as many — 40 percent — reported lower costs. Those declines likely derive from a combination of the added attention being paid to energy efficiency and a reduction in rates in some areas.
The EPA's Reed wasn't surprised to see so many experience a drop in costs. A 1 to 5 percent decrease in energy use is very feasible within a year's time by adapting low-cost strategies, he says.
Popular measures. Conducting energy audits remains the most common energy-monitoring measure, cited by 40 percent, even if many perform them infrequently.
Other strategies used by at least a fourth of respondents include setting energy budget and performance targets and monitoring them annually (38 percent), and participating in Energy Star (29 percent, up from 14 percent in 2006).
When it comes to reducing energy costs, strategies varied. Preventive maintenance, light-emitting diode exit signs, and electronic ballast and energy-efficient lamps are used by at least three-quarters of the respondents. Beyond those, roughly half the organizations also are buying Energy Star-certified products (55 percent), upgrading building control systems (53 percent) or implementing energy conservation programs (49 percent).
"Most people are doing the commonsense stuff now, some of the easy things that consultants were trying to sell us on 15 years ago," says Reed.
About 29 percent are using commissioning or retrocommissioning of buildings and another 33 percent plan to do so within the next two years, figures that Woodin says show that ASHE's efforts to promote it are starting to pay off.
Ongoing commissioning is far more effective than an audit because it is not just a one-time event and addresses the performance decay inevitable over time in engineered building systems, according to Qualk, whose firm conducts such commissioning.
Also telling were the initiatives that the overwhelming majority of organizations surveyed said they had no plans to implement. Those were photovoltaic harvesting systems; replacing conventional power systems with cogeneration, fuel cells, photovoltaic or solar thermal systems; and use of chiller/heater water source heat pumps. The reasons behind the resistance to all three are the cost and the fact that return on investment wouldn't necessarily be immediate, according to Chisholm.
"Those things are not going to happen as quickly as people would like because of the money involved," he says. "Most CFOs don't get excited about spending money unless they can see a return on investment in less than three years. The money is just not there to do it."
Each of five building automation system controls are in use among more than half of respondents: air handlers, variable-frequency drives on pumps/fans, chiller plant optimization, fan/pump speed and boilers. The amount of automation clearly is rising — all have increased since the 2006 survey. But Qualk says the ones that have come into use generally still are underutilized. Steps such as static-pressure reset and temperature resets can go a long way toward saving energy, he says, "because the most efficient system is one that you can turn off."
Other strategies. Three energy-saving design strategies are proving particularly popular in new construction projects: commissioning of building energy systems; integration of low-energy strategies such as building massing and orientation; and "daylighting." Those won't provide anything but a peek at the future for the vast majority of facility managers, however, since new construction has tapered off and just 6 percent of respondents have main hospital buildings that are less than five years old.
Fewer than one in five surveyed organizations (19 percent) is using LEED certifications in new construction. Woodin says many more than that have voiced interest in using LEED requirements without going to the extra cost of getting certified. That shows, he says, that "they're more interested in the output than they are in getting the plaque to put on the wall."
Some slightly different strategies are being incorporated into health care renovation projects to save energy. More than half (51 percent) are using higher-efficiency HVAC equipment, while slightly more than 30 percent are using retrocommissioning and/or reduced-lighting power density and occupancy controls.
Organizations clearly have put more effort into emergency planning in recent years to address energy needs in crises. Asked how energy planning is being incorporated into facilities design to address disasters, 38 percent cite an emergency power system, the same percentage say additional generator capacity and 31 percent mention additional fuel-storage capacity. The impact of Hurricane Katrina and the East Coast power blackout may have turned organizations' emphasis more toward natural disasters.
Fully two-thirds of survey respondents say they participate in a demand-response program, committing to run their emergency generators to alleviate load/stress on the grid. That's an impressive number considering that those programs are available only in areas where utilities have a problem meeting maximum demand.
Another way for hospitals to save on power is to renegotiate their electrical contracts in the retail market to take advantage of excess generation capacity, says Michael Kuechenmeister, FASHE, CHFM, director of plant operations for West Chester (Ohio) Hospital.
That's only possible in states where electricity has been deregulated — much of the Northeast plus a handful of other states such as Illinois, Michigan, Ohio, Oregon and Texas. But Kuechenmeister, whose hospital achieved significant savings by doing so, says many in those states aren't aware that the price of electricity goes up and down just like gasoline does. Due to the economy, he notes, a lot of excess generation is available and that has driven the cost of electricity down.
Proactive steps. Asked to describe innovative energy-management strategies used in their hospitals, organizations indicated they are seeking savings through tried-and-true methods. About 37 percent cited HVAC/air handling improvements, 24 percent said lighting system improvements and 13 percent reported water heater, steam or heat recovery.
ASHE recently recognized 13 health care facilities that reduced energy consumption by 10 percent or more in a variety of ways, but generally by closely adhering to Energy Star guidelines. The winners of the Energy Efficiency Commitment (E2C) awards — Baptist Hospital in Nashville, Tenn.; St. Francis Eastside in Greenville, S.C.; and 11 Memorial Hermann hospitals in the Houston area — saved almost $13 million in energy costs compared with that of their baseline years, and achieved energy savings of 449 million kBtus, reducing greenhouse-gas emissions equivalent to the amount from 17,800 cars.
Leadership is at least as important as expensive new technology in the effort to achieve savings, Woodin says. "No matter what equipment you have, you have to have a dogged person in charge who says 'We're going to save energy.'"
Compiling and coordinating energy-usage information is key, too. Catholic Health Initiatives (CHI) achieved major utility savings from its 72 hospitals spread over 19 states by engaging a bill-paying service — the National Information Solutions Cooperative (NISC) — says Dennis Smith, CHFM, assistant director of facilities services for CHI in Manhattan, Kan.
Relying on NISC and Energy Star Portfolio Manager enables it to identify savings opportunities at hospitals with the highest energy costs, he says. NISC is one of several utility-bill pay services available.
Helping hospitals' missions
The quest for greater energy efficiency is invisible in hospital mission statements. Those stated goals are all about providing exemplary patient care, promoting wellness and serving community needs.
Yet, increasingly, facility managers and others are starting to realize how greater energy efficiency may help hospitals gather the resources to achieve their patient care goals. "For a hospital with a 3 percent operating margin," Reed says, "saving a dollar in energy is equivalent to generating $33 in new revenues."
And it's not just about return on investment. Paul Lipke, senior adviser for energy and buildings for Reston, Va.-based Health Care Without Harm, says more organizations are using many energy tools — available at sites like www.practicegreenhealth.org. They are even estimating their energy-related pollutants' contributions to such illnesses as asthma and chronic bronchitis and even to premature death.
In his group's past dealings with hospitals and health systems, he says, they would rarely mention that energy efficiency was part of meeting their mission to communities. Now, organizations like Cleveland Clinic have embedded energy efficiency and clean energy into their commitment to patient care.
"More people are connecting the dots — from energy efficiency to patient care, health prevention and community well-being," he says.
Dave Carpenter is a Chicago-based freelance writer who frequently covers health care industry topics. Suzanna Hoppszallern is senior editor of data and research for Health Facilities Management's sister publication, Hospitals & Health Networks.
| Sidebar - Energy innovations with an eye on the bottom line |
|
True innovation in energy management comes at a price. Cutting-edge ideas typically don't have the quick payoff that organizations like to see in a tight economy. The hesitance to embrace new energy systems means that older innovations such as microturbines, solar cells and wood-chip incinerators only now are being adopted by health care organizations in any number. Meanwhile, concerns about cost-effectiveness have stalled the acceptance of some new solar applications such as thin film and building-integrated photovoltaic. "We as an industry have a hard time getting our administrations to support energy innovations over capital projects and medical equipment acquisitions, things that will generate revenue," says Delbert Reed, CHFM, SASHE, director of facilities engineering at Ben Taub General Hospital in Houston. "People are under a lot of pressure to reduce costs." Some organizations are pushing ahead as energy innovators, however, even as they keep a close eye on the bottom line. They include the following: Wind turbine. Kadlec Regional Medical Center in Richland, Wash., installed a 5-kilowatt, multidirectional wind turbine that's designed to work at lower wind speeds. After rebate incentives from the Bonneville Power Administration and American Recovery and Reinvestment Act, the cost was $80,000. Kadlec isn't counting on the small turbine for big savings, though. The hospital wanted to showcase a new technology as part of a broad energy-saving plan. "It's not perfected, but it'll take off at some point," says Don Thornton, director of facilities. The demonstration project is one of 10 facility measures that collectively save the organization 30 percent on its electricity, or $250,000. The others include high-pressure steam plant staging and crossover, putting a variable-frequency drive on an existing chiller, a solar photovoltaic array and a lighting retrofit, which provides the greatest single savings at $51,000 a year. Fan-wall technology. Kaiser Permanente is among those to have invested in this concept in air handling, which consists of a multiple-fan array to move air rather than traditional single- or dual-fan HVAC equipment. Daniel Green, project director for MEP and commissioning for Kaiser in Portland, Ore., says the technology was installed there in 2006 and has performed as promised, providing many advantages and advances. The fan wall actually was cheaper than a single-fan unit, he says. The fan-wall technology since has become the standard for HVAC systems for Kaiser programwide. Solar. Sutter Auburn (Calif.) Faith Hospital last year became one of the first acute care facilities in California to have a large portion of its energy demands met by two solar array systems. The two arrays consist of nearly 3,000 solar panels and have a combined capacity of 700 kilowatts, generating more than 1 million kilowatt-hours of electricity per year. The hospital expects to save $2.5 million over the 25-year duration of the project's power purchase agreement with SunEdison, a solar-energy services provider. It remains connected to the traditional electrical grid and has backup generators available in the event of problems with the solar arrays. Wood chips. Cooley Dickinson Hospital in Northampton, Mass., which had operated a wood-chip plant since 1984, upgraded the facility awhile ago. It installed a second wood-chip boiler in 2006 that produces higher-pressure steam, allowing the hospital to install two electric turbines that generate 350 kilowatts of electricity. It also put in a new 680-ton absorption chiller. The net savings achieved by using wood instead of oil are a whopping $2 million a year, according to John Lombardi, director of facilities. "There's a lot of operating costs, a lot of overhead," Lombardi says. "But it's worth doing because of the bottom line and the environment." CHP from brewery waste. Combined heat and power, or cogeneration projects, are increasingly common. But the one used by Gundersen Lutheran Health System in La Crosse, Wis., is unique. Powered up in 2009, it uses biogas discharged from the nearby City Brewing Co.'s waste treatment process and turns it into electricity. The project enables the waste biogas to be captured, cleaned and sent through an engine that Gundersen Lutheran installed at the brewery site. The engine generates electricity that is then transferred to the power grid. And heat generated from the engine is recycled back to the brewery's wastewater-treatment process. Total electricity generated is about 2 million kilowatt-hours a year, about 5 percent of the amount used by the system. |




