Calling all nurses
 Long gone are the days of simple push-button nurse call cables that provide basic communication from the patient bed to the nurses' station.
Long gone are the days of simple push-button nurse call cables that provide basic communication from the patient bed to the nurses' station.
Today's nurse call systems are far more complex and offer significantly more capabilities than their predecessors. As a result, they also require substantially more attention in their planning, design and implementation.
In simple terms, nurse call systems enable patients and clinical staff to summon help with visual and audible signals for routine or emergency needs. These systems also can summon emergency resuscitation teams. Integrating the nurse call system with a staff locator system can identify the location of staff members within the hospital through a central console or special handsets.
The effectiveness of a nurse call system implementation, including how patient calls are answered, can affect patient safety and satisfaction, and nurse satisfaction.
Alarm desensitization is a real problem for today's nurses as different devices (e.g., physiologic monitors, ventilators, infusion pumps and bed-exit alarms) actively compete for their attention. To combat this desensitization, health care facilities should conduct focused, multidisciplinary discussion and planning
sessions before, during and after system installation to address the particular area-specific alarm demands that are placed on staff members.
These planning sessions also should ensure that alarm management is a prime consideration when making functionality and purchasing decisions for a nurse call system.
System requirements
Nurse call systems are required by various codes and are mandated for facilities seeking accreditation by the Joint Commission. As such, these systems routinely are included in the planning and design stage of new hospitals.
The Occupational Safety and Health Administration requires that all nurse call systems be certified or approved by a nationally recognized testing laboratory such as UL. Moreover, some states have specified their own requirements for nurse call systems. Hospitals should check with their state department of health for any regulations that may apply to their area.
Existing systems vary in their degree of expandability. Those having only visual or audible signal displays can, under some circumstances, be modified for voice communication, provided the conduits are large enough for additional wiring.
When planning for new systems, Category 5 computer networking cable seems to be the wiring of choice with most vendors in hospital environments. Many suppliers can custom design systems to interface with other communications systems (e.g., staff registries or pagers).
In addition, some systems interface with admission, discharge and transfer (ADT) systems that are Health Level 7 (HL7) compliant. HL7 is an electronic data interchange standard.
Four major elements
Most nurse call systems consist of the following four major elements:
Central console. In addition to prioritizing calls, central consoles usually display the room number and status of the call. The central console also may track and display the length of time that a call has been in the system — from the time the call is initiated until a room response is indicated. A call reminder feature (if available), usually programmed by the hospital, alerts the attendant if a patient has not received attention within a preÂdetermined time frame. The annunciator, or signaling apparatus, usually is located at the nursing station with the central console and is often out of seeing and hearing range of patient rooms.
Room stations. A room station is a device that can create a signal that can be initiated by patients or staff at patients' bedsides, in bathrooms and showers, as well as in utility rooms and other areas. Call devices come in various designs and many are wall-mounted with push buttons and lights on the faceplate. Pendant-style switches have a push-button switch at the end of a cable, or cordset, that plugs into a jack in the wall-mounted bedside station. Some hospital beds have cordsets mounted on the side rails and provide adapters for interfacing with the nurse call system.
Typical patient rooms will have the following room stations:
- A simple device for patients to call for assistance from their bed (either a cordset or integrated into the bedside rail).
- A push-button, wall-mounted plate at each bedside to allow caregivers to call other staff or announce emergency situations (e.g., staff assist or Code Blue).
- Pull-cord stations in a patient lavatory to alert staff to a request for assistance or emergency situation.
Hallway communication stations. These are strategically placed stations that allow caregivers, who may be in remote or isolated locations on their unit, to be notified of calls. They can be designed to show which patient is calling or only have the ability to communicate with the front desk, with no display to ensure patient confidentiality.
Corridor or intermediate station lights. These types of lights are located outside patient rooms and corridor intersections and are illuminated when calls are signaled, to assist the staff in locating the calling room. The call signal is relayed to the central console, which triggers an audible tone and a display of the calling room number. Signals from bathrooms and showers trigger tone and light signals (usually pulsating) that are different from the calls from beds, because lavatory calls may require more immediate attention.
Enhanced system options
Beyond traditional nurse call systems are enhanced, or microprocessor-based, systems. Their central consoles can be preprogrammed to hospital specifications or they can be user programmed, which permits staff to enter the name, room number and medical data of each patient.
The following attributes should be considered when looking at an enhanced nurse call system:
Interfacing to the hospital information system (HIS) and ADT system. Today's enhanced systems can interface with the HIS and ADT system to allow access to patient-identification information.
With these enhanced nurse call systems, caregivers can be assigned responsibility for specific patients or rooms through the master console. Thus, when a patient places a call, the system can either display the names of the assigned caregivers on the console or direct the call to the appropriate caregiver.
This helps to identify the appropriate person to respond to the call, and some systems also will display and forward the patient call directly to a radio pager or wireless phone number, if available. A few systems even display a graphical representation of the floor layout that shows, for example, the patient's name and status along with the names of any caregivers in the room.
Integrated staff/equipment locator options. The nurse call system also may have an integrated staff locator system — an infrared (IR) or radio-frequency (RF) transmitter badge, wristband or similar device that wirelessly communicates with an installed locator detector.
Detectors, which often are incorporated into the room stations, can transmit staff or equipment-identification information to the nurse call system. These detectors also may be located in the ceiling or elsewhere in the structure of the hospital.
With an IR or RF locator-system interface, the master station may provide a constant display of staff location. With appropriate software, the display may be altered to show the location of staff by job description (e.g., registered nurse or housekeeping). The system also may have nurse-follower capabilities whereby the system constantly senses a staff member's location and routes all patient bedside calls to the appropriate location.
The locator system also can be used to cancel patient calls automatically when a staff member of the appropriate level, or one assigned to the patient, enters the patient's room.
Management and quality-control capabilities. Almost any basic nurse call reporting system can report on calls placed and on time elapsed until a call is canceled. However, a reporting system's capabilities can be expanded dramatically when the system is used in conjunction with an automatic-locator system. For example, the facility can track which caregiver answered a call and how long the caregiver was in the room. It can track response times to ensure adequate staffing. It also can collect data on where individual caregivers spend their time.
The ability to capture and analyze this type of information can prove valuable when planning staffing levels or when evaluating different patient care models. For example, the facility can use the data to monitor the effects of different staffing levels or care models on response times. With some systems, data can be presented graphically (e.g., through the use of bar and pie charts).
Interconnectivity with other devices for alarm notification. Hospitals can interface nurse call systems with other equipment such as bed-exit detectors, physiologic patient monitors, ventilators and infusion pumps to enhance alarm notification from these devices. However, the nurse call system must be preconfigured to connect these devices and there may be limitations in distinguishing each device's alarm.
Many organizations use their nurse call systems to enhance their alarm notification. This may be considered an off-label application for either the nurse call system or device or both.
Often a custom cable connection may need to be created that is not approved for use by the nurse call system or the specific device. If an organization has created or manufactured a cable to connect the device to the nurse call system, the organization then has taken on the responsibility for all alarms being reliably transmitted to the nurse call system. Therefore, the organization also has assumed the liability for correct alarm transmission to the nurse call system and corresponding alarm notification by the nurse call system.
The federal government has its eye on the exchange of medical device data and it is expected that it soon will offer regulations for, and require oversight of, this type of information transfer. The regulations likely will affect not only device manufacturers, but health care facilities that have developed, or will develop, home-grown systems that satisfy the definition of a medical device data system (MDDS). Therefore, it is likely that the health care facility that has developed an in-house system will be subject to the proposed MDDS ruling as if it were a medical device manufacturer.
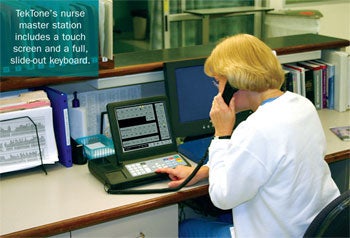 |
| TekTone's nurse master station includes a touch screen and a full, slide-out keyboard. |
Purchasing considerations
Many organizations are considering interfacing bedside equipment with their nurse call systems to enhance alarm management. But without proper communication and planning among caregivers prior to the integration, what started out as alarm-management safety enhancements could devolve into alarm desensitization and fatigue.
Selecting the proper team (e.g., nursing staff, information technology and biomedical engineering personnel) and having them review the features of a new nurse call system are essential to its success. Without buy-in or acceptance from nurses or other staff members who may resist change, the system will fail no matter how well-conceived or implemented.
To overcome this, staff members should be involved early in the evaluation and selection process. The equipment purchasing team should consider the staff's needs and concerns when making decisions. If nothing else, the medical staff will know that their input was sought and valued. It is more likely, however, that nurses and others who are most aware of day-to-day patient care operations will be in the best position to guide decision-making.
As with other new programs (such as patient-safety initiatives), selection of one or more champions on the staff can be extremely beneficial to system implementation and staff buy-in. These representatives will be in the best position to explain to their colleagues how proposed systems can affect their jobs and lead to potential patient care improvements.
Once systems are chosen, staff must be fully trained as part of the system's implementation. Suppliers typically will provide some training for facility staff who then are responsible for training other users. The amount and timing of supplier-provided training usually is negotiable and purchase committees should discuss options with each supplier.
Initial training should allow sufficient time for staff to become comfortable with the system and have their questions answered. Supplemental training may be necessary as users become familiar with the systems and develop new questions about various features. Facility managers also can identify areas where follow-up training is necessary by monitoring staff response times and other data and reports generated by the systems.
Health facilities considering the purchase of an enhanced nurse call system also should take the following steps:
- Contact the state department of health for more information on local nurse call system requirements.
- Address interconnectivity, alarm notification processes and wireless communication devices (e.g., phones and pagers) as part of the planning process.
- Consider standardization of audible and visual cues for different levels of alarms and protocols for notification and response to the calls from the system.
- Incorporate data recorded by systems in conjunction with patient and family feedback as part of the facility's overall quality-improvement activities.
A patient lifeline
It's no exaggeration to say that a fully functioning nurse call system is a lifeline between the patient and the hospital's clinical staff. With careful planning and selection, health facility professionals can help strengthen that lifeline. HFM
Mark Meyers, R.N., NE-BC, is senior associate in the Applied Solution Group at ECRI Institute, Plymouth Meeting, Pa. He can be reached at mmeyers@ecri.org.
| Sidebar - Interfacing nurse call systems with handheld communications |
| For the most part, the primary handheld communication devices used by nurses in the health care environment are pagers and wireless telephone systems. When a nurse call system is interfaced with a radio-pager system, pages can be initiated either by the attendant using the master console (attended mode) or by the patient activating the call button (unattended mode). A combination approach also can be used. Typically, these systems are configured so that pages for a specific patient or bed are directed either to an individual caregiver's pager or to all the pagers in a pager group — which may consist of, for instance, the personnel on the patient care team (i.e., a nurse) assigned to that patient. Although pagers with simple numeric displays may be used, enhanced nurse call systems typically are used with pagers that have large alphanumeric displays containing at least 32 characters. These pagers allow details about the call to be communicated along with the page. Through use of predefined alphanumeric messages, caregivers can determine the urgency of a call and the appropriate action to take before going to the patient's location. When utilizing a pager system, ensure that the system capacity is sufficient to handle the volume of nurse call notifications. Overloading the paging systems may cause delayed or missed pages. When incorporated into nurse call systems, wireless phones provide the same alphanumeric display capability of a pager system, but also allow the caregiver to use the phone to speak directly through the nurse call intercom with the patient or the attendant at the master console, including being connected as extensions of the facility telephone system's private branch exchange (PBX). Full-function integration will, at times, allow caregivers to fulfill a patient's request without leaving their current locations. Caregivers also can use wireless phones to keep in touch with physicians, other caregivers or a patient's family members. There are three common methods of providing wireless telephone service. One is using wireless phones to connect to the hospital's PBX. This is similar to a wireless phone used in many homes. Voice over Internet Protocol is another method of wireless phone communication that utilizes a hospital's wireless infrastructure. The last method is to use a distributed antenna system. This equips a facility with an internal wireless network similar to a cellular phone network. Careful planning is required before a wireless telephone system is deployed to ensure that the system will not adversely affect other wireless devices and systems, that it will provide adequate coverage and that it will be of sufficient quality and reliability. Facilities that use the technology must address these issues to ensure the confidentiality and reliability of voice communications. |
| Sidebar - Remote monitoring adds twist to patient communication |
| While not directly related to the communication infrastructure of nurse call systems, remote patient monitoring is growing in interest as another way for caregivers and their patients to stay in touch, especially in situations where patients can be monitored from home. For conditions that have traditionally high readmission rates, such as diabetes and congestive heart failure, the technology for remote patient monitoring is becoming critical to managing patients' care and keeping them out of the hospital. Home-based health monitoring technologies have evolved greatly since their inception in the 1970s when medical-alert systems enabled patients to alert a call center after falling or while experiencing chest pains. Today's sophisticated systems include monitors, clinical information databases, Internet-based decision support tools, health-management programs and content-development tools. Nonetheless, remote management of patients by telephone or e-mail historically has a poor reimbursement track record in the United States. Reimbursement may improve, however, because the American Medical Association established eight new Category I Current Procedural Terminology (CPT) codes to facilitate reimbursement effective January 2008. These include CPT codes for telephone assessment and management and online evaluation and management of an established patient. Interoperability is also a key part of patient monitoring, both on-site and remotely. However, the lack of progress in creating electronic health records stymies integration of clinical data for access by care providers. Expanded home-monitoring capabilities using the Internet for such data as blood glucose levels and blood pressure readings, have been developed by some manufacturers in an effort to cut treatment costs while improving a patient's quality of life. Candidates for home monitoring are patients who are well enough to be discharged but whose chronic conditions necessitate close follow-up to prevent frequent hospitalization. |




