Steamed up
 As a recommended practice standard that provides guidelines and recommendations, the American National Standards Institute/Association for the Advancement of Medical Instrumentation ST79 Comprehensive guide to steam sterilization and sterility assurance in health care facilities is an all-encompassing standard covering everything from workflow through the sterile processing department (SPD) to instrument identification and traceability.
As a recommended practice standard that provides guidelines and recommendations, the American National Standards Institute/Association for the Advancement of Medical Instrumentation ST79 Comprehensive guide to steam sterilization and sterility assurance in health care facilities is an all-encompassing standard covering everything from workflow through the sterile processing department (SPD) to instrument identification and traceability.
Revised in its 2010 edition, it gives recommendations of a "should" nature. According to the standard, "'Should' indicates that among several possibilities one is recommended as particularly suitable, without mentioning or excluding others, or that a certain course of action is preferred but not necessarily required, or that (in the negative form) a certain possibility or course of action should be avoided but is not prohibited."
Health facilities managers and design engineers need to be aware of key recommendations in Section 3 of the standard, which covers design considerations, and how the 2010 recommended requirements apply to their own steam sterilization systems.
Steam quality
According to the standard, "There are two common sources for steam used for sterile processing: hospital steam boiler systems and self-contained electric boilers. In both cases, a treated water supply is necessary to remove total dissolved solids (TDS). Each system should be designed, monitored, and maintained to ensure that the quality, purity, and quantity of the steam provided are appropriate for effective sterile processing."
The standard describes steam quality as having three parameters: dryness, non-condensible ratio and superheat. It gives acceptable levels for those three parameters, and states they should be assessed and documented "upon installation or relocation of the sterilizer and after any change to the steam distribution lines or boiler supply water." The standard also suggests day-to-day monitoring and alarms.
Steam dryness is a measurement of how much liquid water is present in the flowing steam. It is expressed as a "dryness fraction," which is a percentage by weight. The standard states, "Steam dryness should be between 97 percent and 100 percent." This dryness fraction is measured at the inlet to the sterilizer. Most boiler plants do sampling of the steam near the boiler header to measure dryness.
A sample cooler in the boiler plant typically condenses some steam from the header or main to measure solids and pH. If liquid is being discharged by the boiler as carryover, it shows up as a high solids concentration. The same measurement normally can't be used at the sterilizer. Instead, a calorimeter test is used. Liquid water at the sterilizer might be boiler carryover, but also can be condensate. Condensate is the equivalent of distilled water and will not have high solids.
If too much liquid water flows into the sterilizer chamber, a "wet load" may result. Any liquid water present on or in the sterilized container means it must be reprocessed. This is often a three-hour procedure. The liquid water can breed bacteria and become a threat to patient safety. Sometimes the wetness isn't discovered until containers are opened in the surgical suite. Then, reprocessing becomes an emergency and all other items processed with the wet load are recalled.
Steam usually is delivered to the SPD at 60-90 pounds per square inch (psig) gauge. Unlike most other hospital processes (except humidification), the steam is injected directly into the sterilizer. This makes the SPD one of the first to know if there is a steam system upset.
The sterilizer is designed to deal with the instruments being soaking wet. The steam is supposed to condense on the instruments and that is what creates the "time and temperature" required to achieve sterilization. The drying cycle is programmed to pull a vacuum, which causes the condensation to re-vaporize. When too much "extra liquid" is carried with the steam, the dry cycle can't handle all the liquid and wet loads will result.
The standard defines noncondensable gases (NCGs) as "gases that cannot be liquefied by compression under the conditions of temperature and pressure used during the sterilization process." In practical terms they are air, carbon dioxide (CO2) and oxygen (O2).
"Air" means the atmospheric air that is introduced to the sterilizer chamber when the door is opened or into the steam piping when the system is opened for maintenance. The steam system normally loses water over time due to leaks, humidification and boiler blowdown (flushing the boiler). The system needs some fresh water to make up for these losses. Air is introduced into the system with this fresh makeup water, as well as carbonates (CO3), which are the primary source of NCGs.
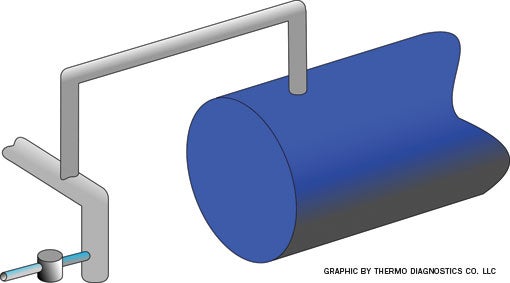 |
| Usually the largest pipe in the steam system, the boiler header removes liquid water carryover before it can reach the sterile steam supply. |
When heated in the boiler, the carbonates break down producing O2 and CO2. These two gases can cause problems with corrosion. Boiler treatment adds chemicals to the system to try and head off the corrosive negative impacts of CO2 and O2. The boiler water pre-heater or deaerator tank are designed to remove dissolved air and NCGs from the boiler feedwater.
The standard states, "The level of [NCGs], expressed as a fraction by volume. [NCGs] (e.g., air) should be at a level (less than 3.5 percent [volume/volume] condensate) that will not impair steam penetration into sterilization loads." So the steam dryness is a weight ratio of liquid to vapor and this is a volume ratio of gas to condensed steam (liquid).
Air and NCG problems
Air and NCGs cause problems with the sterilization process in two specific ways. First, they lower steam temperature; and, second, they take up space, insulating the instruments that are meant to be heated and sterilized. The lowered steam temperature occurs because there is a mixture of steam and air as opposed to pure steam. At 30 pounds per square inch (psi), steam is supposed to be 274 degrees Fahrenheit (F). If the mixture is 10 percent air, the temperature will fall by 7 degrees F. At 30 percent air, the temperature falls by 22 degrees F, and at 50 percent air the temperature is reduced by 49 degrees F. The more air present, the harder it becomes to reach the 270 degrees F required by the sterilization cycle.
During a sterilization cycle, steam flows toward the instruments and collapses and condenses as it transfers heat to the instrument. The steam flow also pushes air and noncondensible gases toward the instruments. Visualize wind pushing balloons (NCGs) toward the surface of the instrument. Since they do not condense, they can collect at the instrument surface and create a heat transfer barrier.
Air is a very effective insulator — 0.01 inches of air is the same barrier to heat transfer as 15 inches of steel or 11 feet of copper. Recall that it is the time, temperature and condensing action that causes sterilization. The sterilizer removes these gases during the cycle using pulses of steam and either gravity or a vacuum pump to evacuate air and NCGs.
The standard states, the frequency of use for a Bowie-Dick test: "For routine sterilizer testing (dynamic-air-removal sterilizers only), should be run, within a test pack, each day in an empty sterilizer before the first processed load." Then, throughout the day, "biological indicators" are placed at strategic points to confirm the steam penetration. If the steam system is delivering air or NCGs, either one of these test devices can show a failure. Once again, this makes the SPD one of the first to know if there is a steam system upset.
Superheat is steam that is hotter than saturation conditions, and so condensation cannot occur. It is an unsuitable medium for steam sterilization. The standard calls for measurement of superheat of steam expressed as a temperature in degrees above saturation point. This value should be less than 77 degrees F. Superheat can be found in large campus systems or district (city) steam by design. It also can be the result of a large reduction in pressure through a pressure-reducing station. It is unlikely to be of significance in the circumstances normally encountered in hospital steam distribution systems, but superheating might arise if the main steam supply pressure is unusually high, about 250 pounds psig or more. Superheated steam can cause failure to sterilize, scorching of textiles and paper, and rapid deterioration of rubber. Once again, the sterilizing cycle creates wetness and superheat prevents wetness.
Sterilizer manufacturers specify a minimum pressure they need to operate and sterilize effectively. This is measured as steam pressure during peak steam flow. The standard also addresses this in the design section "Steam Quantity." According to the standard, "Total steam demand and the corresponding necessary capacity should be determined so that the steam supply system can be designed and built to meet the peak demands of the facility. This information should be used to ensure that constant steam pressure (meeting the manufacturer's recommendations for minimum pressure) is available at all times and under all conditions of steam demand to properly operate sterilizers.
In general, there are two symptoms of low steam quantity. First, the sterilizer will go into alarms, especially door seal alarms found on newer sterilizers. Second, wet steam issues can happen sporadically and with no rhyme nor reason. High pressure drops are proportional to high velocity, causing condensate to flow past trap stations. Sudden pressure drops can impact trap performance and responsiveness. Many facilities have added pressure transducers to the sterile steam supply to monitor the steam pressure remotely.
Treatment chemicals are addressed under steam purity. According to the standard, "Caution is advised in the use of amines for conditioning steam lines (as opposed to the use of amines in feedwater treatment) because amines can stain packaged items within the sterilizer." The injection of amines directly into the sterile steam supply can create the staining issue, as well as high pH if the pump were to overdose the line. Most condensate formed in sterilization is not returned anyway, so there is only a small condensate load compared with that of the rest of a health care facility.
Regarding monitoring and alarms, "Procedures should be in place for the preventive maintenance, repair, and monitoring of boilers and steam distribution lines that provide steam for sterile processing and for the documentation of corrective actions." This means that a pressure monitor is a good idea, and that traps and insulation on the sterile steam supply should be "hyper-managed."
Most facilities check traps to find the energy loss created by leaking valves. On the sterile steam, they should be more concerned with traps that have failed closed or have plugged. Going back to the previous wet steam and boiler carryover discussion, recall that boiler carryover has a high solids concentration. These solids are small enough to go through strainers. They can plug traps from the downstream side since the 60 psig hot water "flashes" when it drops in pressure at the trap outlet.
For this reason, temperature monitoring of traps on the sterile steam supply is a good idea. It can be as simple as regular surveying with an infrared thermometer gun or more sophisticated with a wireless transmitter system. Regarding the prevention of boiler carryover, the standard states, "The monitoring and testing program for boilers should generally include determination of: a) incoming water hardness, pH, iron content, and alkalinity; b) boiler water alkalinity and pH; and c) condensate return alkalinity, conductivity, sulfites, and pH." Facilities professionals also should test the boiler water conductivity or TDS.
Maintaining quality
The revised standard suggests ways to ensure that the quality, purity and quantity of the steam provided are appropriate for effective sterile processing.
To maintain this quality, health facilities professionals should follow these steps:
- Perform a steam quality validation whenever a sterilizer is relocated, steam piping changes are made to the sterile steam supply, or boiler water supply systems change. Values to be tested are dryness fraction, NCG level and superheat.
- Monitor steam pressures, trap operation on the sterile steam lines and water chemistry (incoming, boiler and condensate return) on a continuous basis.
- Consider a proactive communication strategy, so the boiler plant staff is calling the SPD to notify them of a steam system upset, instead of the other way around.
Facility professionals must be proactive. The revised standard will be in most SPDs and it will prepare them to effectively question these aspects of the steam supply.
— Walt Deacon is president of Thermo Diagnostics, West Lafayette, Ind. He can be contacted at wdeacon@thermo-diagnostics.com.




