Just right
Health care delivery is changing. The baby boomers are aging and demanding a higher standard of care than their parents did. Concurrently, the total hospital square footage per patient bed has been increasing — and construction costs have, until recently, been rising. These two trend lines are untenable in today's market and going forward.
Health care architects must ask themselves: "Have hospitals gotten too big?" and "How can we design better facilities geared toward a consumer-oriented society with less capital, given the current and projected economic climate?"
Architects cannot abandon the positive strides that many worked hard to achieve over the past few decades. But they need to think about how they can develop a smarter design process that addresses the initial capital constraint issue, delivers more efficient hospitals, reduces long-term operation costs and creates convenient hospitals that consumers demand.
The rightsizing process
Health care providers have been validating "Lean" practices to operations for years. Likewise, health care architects should apply these tenets when designing and building health care facilities.
While working with clients, designers need to take a second look at the overall operational model of care, work-flow analysis, patient throughput, staff efficiency, staff and patient safety concepts and many more additional variables in the health care delivery equation.
The multidisciplined design team — which includes thought leaders such as strategic planners, functional planners, programmers, architects, engineers and other design consultants — should consider research and evidence-based ideas to understand complex problems. When applied, these studies can improve patient flow, minimize walking distances, provide multifunctional adaptable space, implement standardization and improve sustainability. This leads to functional and elegant design solutions.
The goal is fine-tuning operational effectiveness and rightsizing square footage without sacrificing the customer experience.
Mission and goals
Before beginning, the design team needs to fully understand the health care system's mission and goals. What is the system's model of care? What kind of services is the system providing? What is right for the community? What is profitable for the business?
After answering these questions, discussion can begin to define the most efficient and productive ways to incorporate these services into the design.
The key is to optimize space for staff and operational efficiencies, embrace Lean concepts to streamline work flow, integrate research and evidence, assimilate emerging information systems and medical technologies that streamline processes, integrate patient safety and infection control principles, create benchmarking processes, analyze designs and eliminate wasteful processes.
It's possible to do all of this by rightsizing the facility — creating a facility that fits the need, incorporating operational efficiencies and working with the integrated design team to plan and build the facility quicker with fewer errors and omissions.
Operational strategies
 |
| Separate circulation patterns for staff, patients and materials improve work flow at Hualapai Mountain Medical Center is Kingman, Ariz., which was designed in associatoin with Desgin Stuido Inc. |
Beyond the physical manifestation of the design are operational strategies. Designers must understand these and help define them before embarking on the design process. Building teams have to streamline processes that, in turn, produce efficiencies. When examining an appropriate operational model of care, it is essential to have a pilot program of this new model in the existing hospital before moving into the new one.
The model should include the following tenets:
Incorporate evidence and trends in health care design. The team should distinguish the difference between "evidence exists," "trends under study" and "trends not examined."
Develop a medical record or electronic chart protocol that provides a Lean process. There are many software and hardware packages available today that help to streamline processes, minimize errors, enhance patient safety and create a more efficient and satisfying patient experience.
Use a just-in-time delivery model for all support services. This will allow the materials management department to be much smaller as the space needed to store supplies is greatly reduced. The smaller footprint allows for a more efficient overall structure and brings parking and vehicular circulation patterns closer to the building.
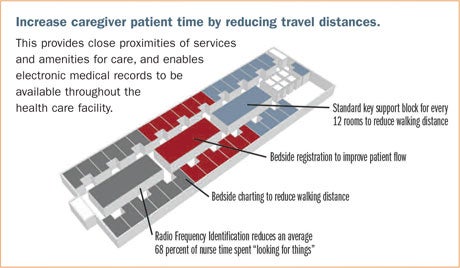
Increase caregiver-patient time by reducing traffic distances. Decentralized nursing stations, decentralized medications and decentralized storage spaces allow caregivers to be closer to the patient room and the point of care. Nurses walk an average of five miles in an eight-hour work shift. Thoughtful designs can help cut this walking distance in half, allowing the caregiver to spend more time at the patient's bedside.
Integrate smart technology. Bedside registration can help streamline operations of the hospital, create a more efficient patient process and reduce unnecessary space in waiting and registration areas. Explore using electronic records, an integrated medical and clinical chart and bedside registration as much as possible to enhance patient flow and efficiency of the flow, minimize charting errors and inaccuracies and potentially eliminate space within the hospital for registration altogether.
Employ a hospitalist strategy to increase throughput efficiency. This strategist acts as an organizer of patient information flow, helping to integrate the patient's care from initial registration through release.
Learn from other industries. For example, the health care design community can learn something from the
aviation industry in understanding how standardized design of repetitive spaces such as operating, imaging, intensive care unit (ICU) and acute care rooms, can help enhance protocol behavior, aid in patient safety through the elimination of errors, and enhance the ease and speed of facility construction.
Efficient flow
Compatible adjacencies and efficient flow designs help staff focus on productivity. It is important that the caregiver be located as close as possible to the patient's bedside. Distractions need to be minimized to increase patient safety and caregiver attentiveness. A simple design improvement can increase a hospital's room turnover rate.
Other concepts to consider include the following:
Integrate one floor each for all interventional and noninterventional activities. This design creates efficient patient flow and reduces unnecessary staff and support space.
Co-locate waiting areas. There is no need for redundant waiting rooms for imaging, surgery and cath labs. One waiting room can be included for interventional activities and another for noninterventional activities.
Don't separate rooms for pre-op and post-op. Treatment and patient rooms used for morning pre-op patients can be used by post-op patients later in the afternoon. It's the same space, just utilized differently.
Design surgical prep-and-recovery rooms adjacent to the emergency department. This will allow a "swing" use of these rooms during opposing peak hours. This also will reduce the overall square footage of the hospital and create a more efficient building footprint.
Share support space between related adjacent departments. For example, design a block of support space between an ICU and post-anesthesia care unit (PACU) to allow for the opportunity to share this
co-located support space between the two departments. This not only saves overall square footage but also simplifies restocking patterns while creating a more efficient support model. Design the emergency department next to the diagnostic and imaging department, allowing shared use of the computerized axial tomography (CAT) scan and other diagnostic procedures.
Separate circulation patterns for staff, patients and materials to improve work flow. Allow for two corridors — one for staff and another for the public — to eliminate incompatible circulation crossovers and allow for a more efficient work flow process.
Plan for flexibility
 |
| Decentralized nurses' stations, medication, and office and storage space puts caregivers closer to patients at Texas Health Presbyterian Flower Mound. |
Flexibility is still the mantra of hospital design. A health care facility's medical requirements and model of care determine the building's design and, ultimately, its geometry. Successful design solutions include built-in, long-term flexibility concepts that allow facilities to change and grow over time in a more cost-effective and graceful manner.
Other ideas to consider include the following:
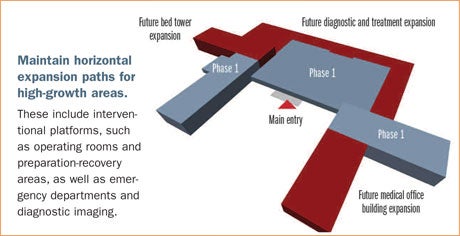
Allow modular growth. Building expandability involves the ability of the original structure to grow in an orderly manner, ideally along a well-conceived, understandable and expandable infrastructure. This will give the facility a more functional and responsive life to suit the ever-changing model of care.
Have clear separation of fixed and flexible elements. This will increase the building's ability to adapt to new demands. Fixed elements include vertical circulation in elevators and stairways, major horizontal circulation corridors, nonmovable equipment, toilets, mechanical/electrical/telecommunication rooms, and structural components such as columns, shear walls, diagonal bracing and so forth.
Allowing the building to respond to the ever-changing health care delivery landscape is a much more efficient and less costly alternative to building new structures at a later date — a concept that will be even more important as we move into the future.
Incorporate a straightforward circulation system. Such a system should delineate a separation between public and service traffic while providing a chassis for future incremental growth. Circulation corridors should be planned for easy and quick expansion, locating large, complicated modalities such as magnetic resonance imaging and computed tomography outside of the planned growth path.
Create a planned growth concept. This utilizes a plug-and-play approach to flexible growth by developing a circulation system that includes a central service and circulation chassis surrounded by a diagnostic and treatment "warehouse of flexible space." The outside location of these components will simplify renovation at a later date to meet changing patient needs while allowing the important infrastructure elements to remain intact during renovation.
Program and plan for swing use of space during opposing peak hours. For example, health care systems can use ambulatory care unit facilities for after-hour emergency department use. When patients enter the hospital for surgery, they can begin and end their treatment at the same place. A patient is admitted, taken to pre-op next to the operating room, and then into the PACU for recovery. That same patient pre-op area turns into a post-op area later in the day, where the patient returns full circle.
Design larger, uninterrupted structural bays into the facility. These can accommodate renovation adjustments to modality changes and inevitable obsolescence and allow the hospital to accommodate these changes in medical equipment and operational models without requiring a major facility renovation or expansion project.
Incorporate building organizational functions to align with the appropriate structural systems. For example, the diagnostic and treatment blocks should be designed with open, flexible, long-span structural systems, while the patient units are more specific, short-span, hotel-like structural configurations. This will promote ease of renovation and allow for greater flexibility.
Allow surge capacity and scalability for seasonal or disaster flexibility. This concept focuses on three goals: scalability that conforms to fluctuating patient volumes, medical consequence management to allow for continued operations in the midst of unknown catastrophic events, and threat mitigation to minimize the event of intentional explosive devices, harmful agents or natural disasters.
Efficiency first
In today's fiscal environment, hospitals can no longer afford to develop facilities that are constantly increasing in scope and on a path to unlimited size and cost.
The current climate of health care reform will require efficiently designed and operationally Lean facilities that continue to embrace flexibility and adaptability to future changes. Smart architects will deliver operational effectiveness and right-sized square footage without sacrificing patient safety or experience.
For facilities owners and operators, this means an improved financial model and increased bottom line as well as improved patient outcomes in environments that support healing.
Dan Noble, FAIA, FACHA, LEED AP, is executive vice president, and Angela Lee, AIA, ACHA, LEED AP, is senior vice president, at HKS Inc., Dallas. They can be contacted via e-mail at dnoble@hksinc.com and alee@hksinc.com, respectively.
| Sidebar - Strategies for inpatient units |
| If recognized and implemented early in the facility planning process, the following inpatient unit design strategies can save time and money as well as help promote better patient care: • Organize inpatient units to specific patient acuity, enabling improved staff efficiency, better patient safety and more efficient space. • Design acute care inpatient units to be 575 square feet per bed, and patient rooms to be 270 square feet each. This will accommodate either a centralized or decentralized nursing model. It also will minimize family waiting in units with all private rooms. A 36-bed unit works with a variety of staffing ratios. • Use a racetrack configuration, which offers efficiency as well as easy wayfinding. The configuration provides the most efficient perimeter-to-core ratio and enables direct corridor sightlines for caregivers and patients. It also promotes separation of public and service areas • Design an appropriate structural system for patient units. Align the first floor height with the diagnostic block for future expansions.
|
| Sidebar - Strategies for Medical office buildings |
| When designing a medical office building (MOB), health care architects should review all potential options to maximize space and cost efficiencies, including the following: • Place the hospital administration and outpatient functions on an upper floor for cost savings, leaving hospital lease space on the first and second floors. • Locate administration and outpatient services in an attached MOB to use less-expensive space, create a more efficient diagnostic and treatment block, reduce front-end capital and long-term operational costs, and use less space for a more efficient deployment of full-time equivalent employees. • Locate the medical office building core to allow for different operational models, maximizing the number of potential lease spaces and offering flexible clinical models for different practices. • Use a 28-foot-by-30-foot grid leasing model, which provides three 9-foot-by-4-foot spacing modules with one structural bay. Also, use single-tenant and multi-tenant lease depths, offsetting the core for greater floor flexibility. • Apply a 28-foot-by-30-foot grid for an MOB clinic model, using on-stage and off-stage concepts. This efficient clinical space layout provides flexibility for different physicians' practices with the same space at different times.
|
| Sidebar - Strategies for Diagnostic and treatment buildings |
| Diagnostic and treatment buildings should use the following strategies – which reduce duplication of key spaces as well as share support services and staff – to allow future expansion without interrupting ongoing operations: • Locate soft space near high-growth areas for expansion. The front door should never change. However, high-growth areas, such as surgery, imaging and emergency, should be strategically sited for future growth. • Make sure ancillary departments, such as materials management, dietary and the loading dock, have room to flex as high-growth areas expand. • Strategically align HVAC zones with smoke compartments. Organize smoke zones so that one air-handling unit serves each zone, minimizing the need for smoke and fire dampers. • Design an appropriate structural system for diagnostic blocks that will increase the speed of construction, allow long spans for flexibility, enable better coordination between trades and provide flexibility above the ceiling for future changes.
|