Senior settings
 A facility that is properly constructed to meet the needs of a patient also serves as an integral part of patient care. If the facility is less than an optimal caregiver, it could contribute to stress-creating conditions, medical errors and extended lengths of stay. This is especially true for elderly patients, who are sensitive to disruptions and, in the case of those with symptoms of dementia, easily disoriented.
A facility that is properly constructed to meet the needs of a patient also serves as an integral part of patient care. If the facility is less than an optimal caregiver, it could contribute to stress-creating conditions, medical errors and extended lengths of stay. This is especially true for elderly patients, who are sensitive to disruptions and, in the case of those with symptoms of dementia, easily disoriented.
Noise — beeps, wheeling carts, shutting doors and alarms that sound in the middle of the night — is a common complaint. And caregiver voices during a shift change can be nothing short of loud and disruptive to patients and frustrating for the families who are staying with them.
Health care planners must understand that verbal communication is going to occur, so it is incumbent on them to create a health care facility that can accommodate this activity. Inquiries should include such questions as: How have users been functioning in their existing facility? Can the environment be changed? Can a noise-creating activity be moved to a more protected location away from the patient? How adaptable to change is the user? Ultimately, a solution as simple as adjusting the paths of circulation away from the patient areas can be derived from such an inquiry.
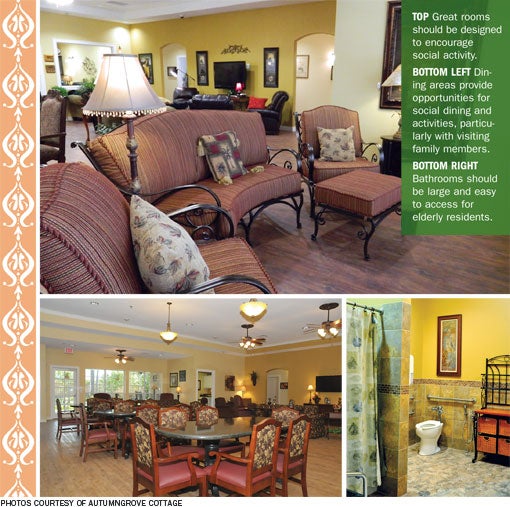
Likewise, positive distractions can be created through careful planning to establish a more stress-free and healthy environment for elderly patients as well as families and staff. Some low-cost options include a pleasing piece of art in a private gathering area, comfortable seating, soothing color palettes, and even music and special lighting to begin creating a calming environment.
More complicated and costly solutions include open, outdoor courtyards and indoor environments that include all of the amenities to which elderly patients have become accustomed.
Of course, consideration should be given to the environment of care for a staff member as well as for a patient. He or she is being affected by the same noise, lighting and stress distractions as is a patient. Thoughtful design of patient care areas can give the clinical staff a positive place to work as well.
Variety of environments
Many of the aforementioned design touches don't sound like a health care facility at all. However, they are some of the approaches senior care facilities are using to reduce stress on families, staff and patients.
Hospitals that are seeing more elderly patients, as the baby boom generation reaches its senior years, can take note of these and similar design trends. Many can be incorporated into both the critical care environment and the senior facilities in which hospitals are increasingly becoming involved.
Indeed, outside the acute care setting is a growing variety of care environments. In many areas, for instance, the simple nursing home that takes care of a variety of residents is giving way to specialty facilities caring for residents with special needs. Such assisted living facilities give their residents independence while providing the required level of care they need to live the highest quality of life possible. If more intensive care is required, a skilled nursing unit gives this service in more of a clinical environment.
One special residential plan that requires an added level of security but should not ignore the environment of care is that for dementia and Alzheimer's sufferers. Residents in these facilities are affected by their physical environments in a variety of ways.
In fact, the senior care industry is seeing design solutions that evolve away from the hotel- or apartment-style plan to a facility that better stimulates the senses. In these settings with their homelike scale, a less-confusing care environment is created that is more conducive to wayfinding and relaxation, both of which are affected adversely by cognitive illnesses.
These smaller-scale facilities give their residents a feeling of security as well as community. Gardens and private courtyards also are being incorporated into these designs to reinforce the residents' perception of a community.
Small 'villages'
From these concepts, small "villages" are being developed from a combination of home dwellings that can be modified and customized according to the level of care required. The size of these dwellings usually is driven by the economy of scale.
Village designs include controlled courtyards to contain residents who likely will wander as well as areas where others who are more ambulatory can move about freely, having access to open courtyards and gardens. At these facilities, it is not unusual to see vegetable gardens cared for by the residents.
All of this is intended to create a safe environment to which residents can relate from their own homes. Guests feel welcome and the end result is a higher level of interaction between resident and guest and an environment that motivates the resident to go outdoors.
Studies by the Dutch Alzheimer Association have found that nursing home residents spend an average of about 96 seconds a day outdoors and 60 percent of them never receive guests when safety restrictions are in place. By creating communities designed to invite residents and guests outdoors into secure environments, care greatly improves.
The buildings themselves can be used as part of the barrier system, creating natural gardens and health care spaces. Places where residents with or without visitors can go to feel comfortable also can include game rooms and other gathering spaces — even cafes and bistros.
Patients with dementia and Alzheimer's live in a confusing world and behavioral changes are common aspects of the many forms of these medical conditions. Not only is the environment of care for these persons important to help stimulate a positive environment, but to keep them safe so they do not hurt themselves or others.
Reducing confusion
Confusion of place challenges the designer to develop a homelike atmosphere with familiar features. Residents should have an idea of the space's function when they enter. Bedrooms should look like bedrooms and bathrooms, dens and other areas should be easily distinguishable.
Spaces should be distinct, easily identifiable and well-marked with simple signage or symbols at eye level. Surface blending should be avoided and bright, contrasting colors can be used to enhance depth perception and surface changes.
People with dementia have a decreased ability to deal with multiple and conflicting stimuli, and often are overwhelmed when there is too much activity. Thus, acoustical stimulation should be minimized. Public address systems should not be used and noise from institutional equipment should be minimized. Soundproofing, noise suppression and absorbing materials should be included in patient areas to increase privacy.
Although music can be a sobering element in the acute care environment, it is another stimulus that must be considered carefully in the dementia setting. Certain types such as hymns and retro music are calming as are bird songs the first thing in the morning.
Visual stimuli are also important to persons with dementia or Alzheimer's. Glare and bright spots from windows and lighting should be minimized by using carpeting, low-gloss floor waxes and sheer curtains. Pools of light and dark spaces can be provided by using matte finishes and well-thought-out lighting arrangements. When the resident is nonambulatory, views to the outside become increasingly important.
A simple change of environment from a typical nursing home setting to a homelike setting significantly can change the physical and behavioral condition of a patient with Alzheimer's. Being able to sit at a table and see birds at a feeder outside a window and family members moving about can change a senior's disposition and alertness.
The next step?
So, what's the next step? Allowing the residents to stay in their homes and communicate with caregivers electronically? It is being tried, but results of its effectiveness are still being determined.
Whatever the future holds, the senior care environment must create a calming and pleasant atmosphere in which patients can move about safely.
R. Gregg Moon, AIA, ACHA, EDAC, is director of the heath care studio at Kaim Associates Inc. in Kingwood, Texas. He can be reached at gmoon@kaiminc.com. Theresa Strange Johnston, is manager of outreach services for AutumnGrove Cottage, a Tomball, Texas-based chain of assisted living facilities for Alzheimer's care. She can be reached at TheresaJohnston@AutumnGrove.com.
| Sidebar - Special considerations for residents with Alzheimer's |
| Many senior care facilities are not equipped to handle the special needs of their residents with dementia or Alzheimer's, such as protection against wandering. Demand is growing for specialized care custom-tailored to this rapidly emerging segment of the population. There are many aspects that make a cottagelike environment a unique concept, but the two most important differences are size and focus. The smaller size makes a significant difference in quality of care. Following are some of the ways that limiting the size of units to 16 beds provides an effective approach to meeting the needs of someone with dementia or Alzheimer's: Homelike environment. From the moment a visitor pulls into the driveway, a cottage should look and feel like a private home. This homelike environment is one of the cornerstones of the belief that people should be able to age in the same manner in which they are accustomed to living. Personalized care. Caregivers are considered "universal workers." They are responsible for overall resident care, regardless of function. This means a caregiver is involved in all aspects of resident care throughout their day. This allows caregivers to get to know the residents' preferences and provide more personalized care. Deep relationships. Because the smaller units only care for 16 residents, staff and residents get to know each other better. As a disease progresses and a person loses his or her ability to communicate verbally, it becomes critical to know a person well-enough to meet his or her needs. Another benefit to this small size is the deep relationships families form with one another. With the common bond of being impacted by Alzheimer's, family members become friends and often become an informal support group. Offering the smoothest transition from one's own home to one that offers assistance with daily living is important to a person who is confused. Unlike other institutional choices, the cottage concept makes it possible for residents to enjoy the benefits of 24/7 care in a familiar, homelike environment. |




