Practice makes perfect
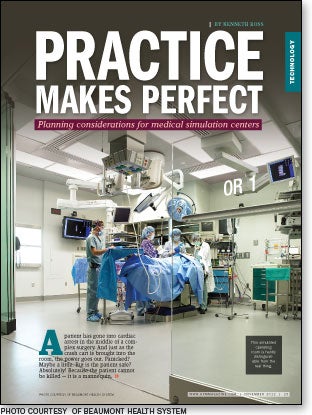 A patient has gone into cardiac arrest in the middle of a complex surgery. And just as the crash cart is brought into the room, the power goes out. Panicked? Maybe a little. But is the patient safe? Absolutely! Because the patient cannot be killed — it is a mannequin.
A patient has gone into cardiac arrest in the middle of a complex surgery. And just as the crash cart is brought into the room, the power goes out. Panicked? Maybe a little. But is the patient safe? Absolutely! Because the patient cannot be killed — it is a mannequin.
And this is strictly an exercise to help clinical staff remain calm and focused during a moment of crisis. Welcome to the world of patient simulation.
The use of patient simulation has been growing as more health care facilities realize the value of training clinical staff in controlled environments. New and experienced doctors and clinicians can practice skills and learn new procedures on advanced mannequins or other training devices. And where better to train new nurses on procedures than in a simulation area away from patients and operating rooms (ORs) that are heavily scheduled?
This inevitably means new projects for health facilities professionals. Over the past 10 years, health care has experienced a five- to tenfold increase in the number of simulation centers, or "sim centers." There are about 1,000 sim centers in the United States and the number is expected to grow. Patient simulation trainers — full-size mannequins (also known as training mannequins or patient simulators) and anatomical models (partial bodies like torsos, abdomens, and arms) — are used to simulate a range of scenarios, from infant delivery to multivictim disasters.
Medical schools were early adopters of medical simulation but, more and more, nonacademic health care facilities are seeing the value of staging and recording events. But why are medical centers spending millions of dollars on these centers? What kind of technologies are involved? And what are the infrastructure and space requirements?
Why build sim centers?
Simulation centers provide a customized learning experience where it's OK to make mistakes. Training can take many forms. It can utilize simulated patients or actors in simulated situations. These are completely different situations but both have a common goal — to create a better prepared medical professional.
Simulation centers are all about practice. Whether training on a simulator or with an actor, there is no better way to learn the skills of working in an OR than practicing in a simulated OR. Likewise for simulated intensive care units (ICUs), emergency departments or other units.
Sometimes, the skills are as simple as opening a sterile pack or learning how to deliver bad news to a patient or family. They're necessary skills, but just not easy to learn from reading a textbook. Simulated environments also allow for coordinated team training and video debriefing, including assessment, immediate feedback and evaluation at the conclusion of the training session. This can be a valuable tool for assessing progress and level of competency.
Simulator use varies substantially. Basic models can help health care providers remain competent in performing intubation skills, basic life support, and advanced cardiovascular life support. Also, hospitals increasingly are turning to simulated operating and labor and delivery rooms with mannequins that help to develop and assess skills for training purposes. With training focused on the simulated patient, sim centers can mimic many circumstances, including realistic challenges like heart rate changes, power outages and specific device failures, such as the shutdown of an anesthesia machine.
Another trend is for simulation spaces to be used for conferences and equipment trials. In some cases, flexible space is being used to build entire operating suites to evaluate the type and position of new equipment.
Complex design task
Establishing and running a state-of-the-art simulation center often requires numerous staff members and millions of dollars. What once was a simple training room has been transformed into a showcase for the hospital and potential revenue source from outside clinicians willing to pay for practice and training sessions.
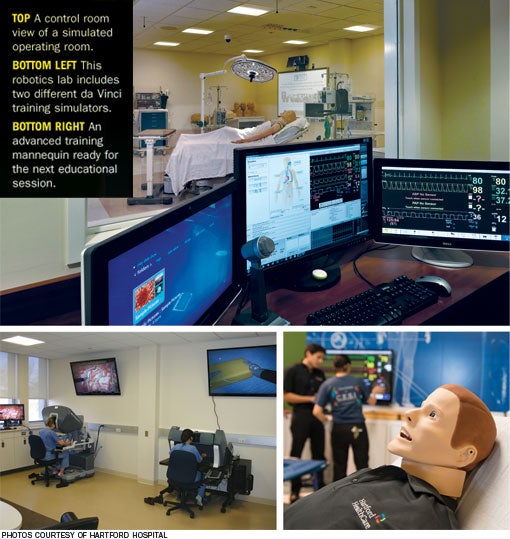
The typical simulation center includes the technology to record, review, score and store the simulation scenarios. This requires not only a staffed control room and robust data storage capability, but a sophisticated network of video cameras, monitors and conference rooms for viewing — similar to audiovisual (AV) control of an OR integration system.
Space and design. As centers have grown, so has the necessity to plan ahead. Simulation centers come in all sizes, from 5,000 to more than 90,000 square feet, and space must be allocated for many different activities. But, deciding how much space to allot for different tasks is challenging. Adding more standardized patient rooms could reduce the number and size of classrooms. Likewise, adding more simulated surgical suites could reduce storage significantly and drive up costs, because each OR typically is filled with actual medical equipment. In the end, knowing the student volume is key to accurate planning.
The four primary physical areas of a health care simulation center include the following:
• Reception and waiting areas. First impressions are important and a hospital must decide whether its simulation center will focus on function or show. For example, if the simulation center is intended to be used for a fee by outside clinicians, the hospital may want a larger, more impressive reception area. In general, reception and waiting areas are used to greet trainees and visitors and often have electronic monitors with schedules and directions. Additional gathering areas will be necessary near skill areas, especially if the center spans several floors.
The hospital may even want to consider adding kiosks or interactive maps if applicable. The size of these areas should assume full operation of the center.
• Skill areas. This is the heart of any simulation center. Whether a full-sized OR, a skills lab or a standardized patient room, these areas define a simulation center. They require control rooms — typically one for each one to two simulation rooms — that are located adjacent to the simulation. They're often behind one-way mirrors with space for monitors, keyboards and microphones.
Standardized patient rooms often can be monitored by one central control room. Depending on the size of the center, users may find one to three ORs, five to more than 40 standardized patient rooms, a fully simulated ICU, imaging rooms and multiple skills labs with four to 20 stations.
If a technology is being used in hospitals — including Sunnyvale, Calif.-based Intuitive Surgical Inc.'s da Vinci Surgical System and various computed tomography scanners — there's a high chance that it can be found in a simulation center somewhere in the United States.
• Teaching areas. No simulation center is complete without classrooms and debriefing rooms. Classrooms are used to teach groups and often incorporate flexibility, such as partitions that can be removed to combine spaces.
Teaching areas need to be near skill areas because they often are used to prep or review with large groups. Some larger centers add auditoriums for large gatherings or boardrooms for more intimate settings in addition to the standard classrooms.
Debriefing rooms typically are smaller and intended to be used by two to four persons to review the exercise personally with a trainee. Often video is played back so trainees can learn from their mistakes.
• Support areas. Hospitals must be careful not to forget the behind-the-scenes spaces that are critical to the support of the educational operations. Simulation centers also include offices, break areas, locker rooms, storage rooms and data centers.
The larger the center, the larger these areas need to be. Some centers have become creative with storage, filling entire walls with large storage units that can house numerous mannequins and other training aids.
Location. The size of a medical simulation center often dictates its location. Small centers can be accommodated in or near the main hospital, but larger centers often dictate alternate sites. The closer the simulation center is to the main hospital, the easier it will be for staff to utilize. If services for visitors are being contemplated, accessibility to parking should be considered.
Other major considerations. Additional key issues that require proactive planning to prevent big problems downstream include the following factors:
• Logistics. Unless a hospital plans to have numerous staff members standing around to direct students, it will need to install a system that directs them to the proper training room. This means monitors in reception areas, waiting rooms, hallways and possibly outside each simulation and standardized patient room.
Medical simulation centers go to extreme measures to ensure that the proper student enters the standardized patient areas and that documentation is accurate, including the use of radio frequency identification tags.
• HVAC load. Facilities professionals shouldn't underestimate the heat generated by the computers, servers, monitors, lights and other equipment within the simulation center space. This load must be accounted for in the overall HVAC system design. Special attention should be paid to control rooms and server rooms, because these areas often are cramped and filled with heat-producing items that are sensitive to fluctuations.
• IT and AV needs. Simulation centers are challenging for information technology (IT) and clinical engineering departments. Computers are needed to run the center, schedule students, schedule standardized patients and reserve mannequins as well as to score the simulations and to debrief the students. Plus, all the systems that run the simulators and other support systems are needed.
Adding to the data overload are the cameras and microphones required to record all of the simulation and standard activities in the center. In most cases, there will be more than one camera per room because of the importance of capturing facial expressions. This means significant amounts of data will be generated each day, regardless of whether high-definition quality is utilized in all areas.
All of the data need to be backed up. Backing up on-site or remotely is critical. The bottom line is that the IT and, likely, clinical engineering departments need to be involved early.
• Future proofing. Like all electronics, the useful life of simulation equipment is limited. Items installed today likely will be obsolete in three to five years. Monitors will break. Computers will need to be replaced. Cameras may need to be updated due to resolution improvements.
The good news is that while there likely will be more pieces of equipment, they tend to be more compact with each successive generation. The trick is to prepare for these changes in technology.
This is nowhere more important than with the cabling. Category 6 cabling will be outdated. Digital visual interface signals will be run over fiber rather than copper. Running conduit in walls — the larger the better, especially if there are 90-degree angles — and providing ceilings with accessible pathways is critical to ensuring that a simulation center remains state of the art. A path for a large, high-speed backbone for remote off-site data backup also should be considered.
Coming into their own
Simulation centers are coming into their own and hospitals are investing large amounts of money to make their centers state of the art.
What once was a 5,000- to 10,000-square-foot skills center began to morph into a 20,000-square-foot simulation center. Then health facilities professionals began to see larger and larger training center projects reach the 50,000- to 60,000-square-foot range. Centers added more and more classrooms and increased the simulated patient rooms past 100.
The sky now appears to be the limit for teaching medical professionals, as a $38-million, 90,000-square-foot facility opened earlier this year in Florida that hopes to train 30,000 to 60,000 medical professionals per year.
Kenneth Ross is senior program manager in the applied solutions group at ECRI Institute, Plymouth Meeting, Pa. He can be reached at kross@ecri.org.
| Sidebar - Medical training equipment commonly found in sim centers |
| Simulation centers, or "sim centers," house a wide variety of training tools ranging from simple anatomical models to realistic simulators. The most common ones include the following: • High-fidelity simulators. Some of the most expensive items found in a simulation center are the high-fidelity mannequins. High-end models can run from $20,000 to $100,000. They continue to be designed more lifelike and are capable of simulating physiologic changes such as a loss of pulse, dilation of the pupils or a sudden drop in blood pressure. Mannequins can be wirelessly controlled by an operator through a computer or a personal digital assistant and may be able to speak in prerecorded sounds or those of the instructor. Custom scenarios can be loaded to provide unique experiences to each training team, such as creating stress that might lead to errors, and data can be collected for performance analysis. • Medical equipment simulators. While simulation centers are full of actual medical equipment, such as that used in an operating room or intensive care unit, users also will find equipment designed specifically for the simulation environment. Since it isn't practical to purchase a $1-million to $2-million da Vinci Surgical System from Intuitive Surgical Inc., Sunnyvale, Calif., on which to practice, hospitals are turning to Intuitive Surgical's $85,000 skills simulator instead. Likewise, ultrasound simulators are convenient because they combine the learning of an ultrasound system with specialized mannequins, providing another type of hands-on experience without the need for live patients. • Models. Simple models are essential in classroom environments. Available as either a full body or specific body parts, such as the heart or the eye, these aids are used to demonstrate anatomy or teach basic skills. • Simulation center software. Software to run a simulation center is equally important. Software can range from basic scheduling programs to more advanced programs to record and score scenario-based interactions. • Task trainers. Typically, the bulk of the items in a simulation center are the task trainers and other basic mannequins for a wide variety of students. Basic mannequins are used for teaching the general public basic skills and cardiopulmonary resuscitation (CPR). Advanced mannequins for CPR, advanced cardiovascular life support and pediatric advanced life support training that provide feedback for improving skills also are common. Besides the full- and partial-body mannequins, users will find specific trainers for such tasks as tying sutures or for inserting an intravenous therapy line. • Virtual reality procedural trainers. Virtual reality trainers also are an important component of the simulation center. These trainers typically are focused on minimally invasive procedures such as endoscopic, laparoscopic, endovascular and urologic procedures. Using realistic hand controls with haptic feedback, students can practice skills like deploying a stent while monitoring patient vital signs and watching a screen, similar to watching a fluoroscopy screen in the operating room. |




