Project integrates care and research in one facility

The five-story, light-filled atrium provides clear wayfinding and natural light, with public-facing waiting rooms on all the floors, giving a sense of connection and belonging.
Image courtesy of ZGF Architects
Mental health is among the most pressing health issues in the world, and yet barriers to care — chronic underfunding, stigmatization, and scarcity of practitioners and facilities — result in nearly half of those in need to forgo treatment.
The new Nancy Friend Pritzker Psychiatry Building at the University of California San Francisco (UCSF), in San Francisco’s Dogpatch neighborhood, seeks to transform this historically underserved area of health care by providing access to mental health services for Bay Area children, adults and families in one facility.
The 166,000-square-foot facility is designed to be UCSF’s first co-location of research and mental health care for pediatric and adult patients, bringing members of UCSF’s departments of pediatrics, neurology, radiology, neurosurgery, psychiatry, anesthesiology and obstetrics/gynecology under one roof to promote collaboration and help normalize the care environment.
Developed by SKS Partners and Prado Group, with ZGF Architects as design architect in collaboration with Perkins&Will, the project will quadruple local access to mental health services while accelerating scientific discovery of improved treatments and prevention.
By treating patients across the full age spectrum, the facility has a unique opportunity to evolve or transition care as a patient ages and help clinicians and researchers better understand physiological and environmental explanations for behavior across a patient’s lifespan.
Project programming
Early on, project partners worked with the health care organization to develop a vision and guiding principles for the Nancy Friend Pritzker Psychiatry Building. One of the critical outcomes of the vision sessions was to create an innovative outpatient mental health facility that would welcome a range of ages and ensure a warm and calming environment where everyone is treated with respect and dignity.
The facility also needed to encompass clinical care, education and dry lab research under one roof. Achieving the vision called for breaking down the barriers between physical and mental health to improve patient care, and developing pioneering, state-of-the art clinical and research services to share and conceive new ideas for preventing and treating mental illness.
Stakeholder charrettes with over 100 UCSF faculty and staff were held to gather program needs, identify synergies across the various practices, acknowledge stakeholder aspirations and fears, and discuss operational approaches to care delivery. The charrette outcomes reflected a patient-centered mental and physical health care setting that emphasized flexible and multidisciplinary spaces to support program goals now and well into the future. The features include:

A dedicated child-friendly entrance creates a welcoming experience for the child, teen and family population.
Image courtesy of ZGF Architects
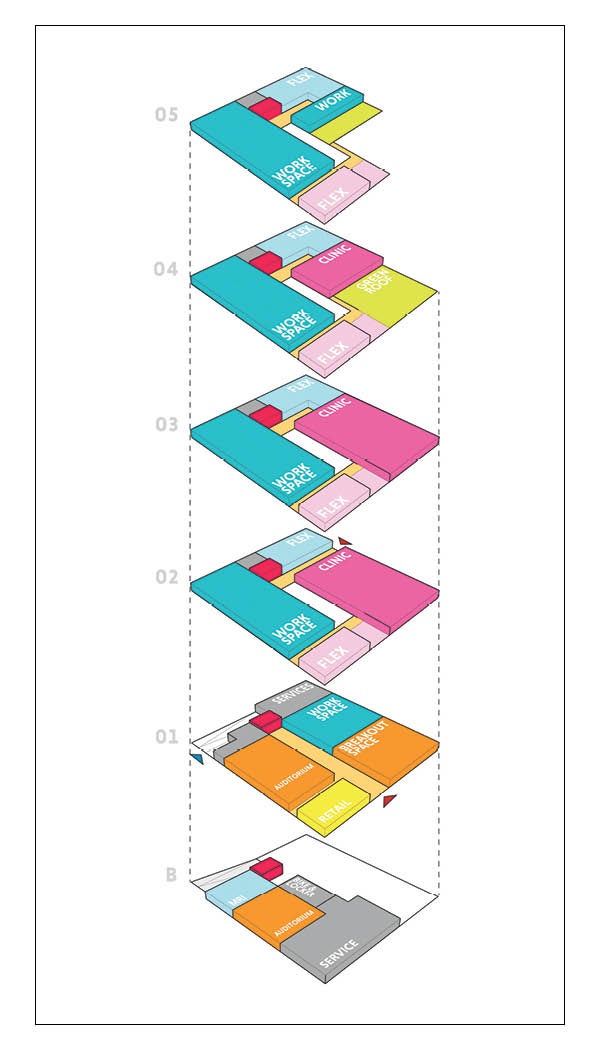
- Two separate entrances to serve patient populations across a range of ages. The building’s orientation on the sloped site allowed for a first-floor adult entrance off 18th Street and a second-story entrance for children and families off Tennessee Street. This provides a dedicated child-friendly entrance while creating a welcoming experience for the child, teen and family population. The program stacking follows suit in separating ages with child and family center services on Level 2, adolescent and family center services on Level 3, adult psychiatry and rooftop garden on Level 4, and executive and administrative space on Level 5. Research labs, bike storage and future magnetic resonance imaging (MRI) services are located on the subterranean level.
- Creating a care environment with patients at the center. Patient waiting rooms are adjacent to the clinical care zones, a key design decision that stakeholders requested. During the design workshops, stakeholders tested various patient and visitor flows into and throughout the building via a process called spaghetti mapping. This exercise revealed that locating waiting spaces at the building perimeter would create more movement for patients and staff. The resulting design improvement shifted the waiting area adjacent to the atrium, placing the patient in the center of the building and reducing travel for both patient and staff.
- Programming that allows for patient care and workplace flexibility. Each office, medical exam room and consulting room utilizes an identical configuration to establish a uniquely flexible integrated care model. Research and clinical spaces are interchangeable for any future needs that arise, while offices have the option of becoming exam rooms or telemedicine rooms for shifting from physical to virtual care. The stacking also allows for flexibility for program growth vertically in the building depending on patient volume and growth over time. After building completion, the program will proceed with building out two MRI procedure rooms, allowing for neuroimaging research to be adjacent to the clinical care program. Each floor contains shared conference spaces to encourage gathering for interactive disciplinary teams, research participant groups, and family and patient consultations as well as open staff workspaces. As many providers will be working between this building and a secondary research or administrative facility, the design includes additional pod space for staff without a dedicated office.
- Integrating clinical, research and medicine with dedicated collaborative space. Stacked vertically and located on every floor, interdisciplinary spaces give opportunity for clinicians, educators and researchers to commingle. The dedicated areas encourage idea-sharing and collaboration to address some of society’s most pressing challenges in prevention and treatment of mental health issues. Private clinical team workspace is located along the exterior wall to take advantage of the natural light. Adjacency to the patient care rooms creates a collaborative space for consultation along with focused workstations. Lastly, research and clinical programming is integrated together on each floor to support a truly multidisciplinary approach to clinical care.
- Auditorium and convening spaces support teaching and the broad exchange of ideas. One of the most critical goals for UCSF is to advance understanding and research beyond the university. The convening spaces support training and teaching between researchers and students, allowing experts to share insights or exchange ideas between psychiatry and neuroscience disciplines, and provide educational programs for patients, family and community members to share and support in mental health.
- Street-level amenities. To increase access and visibility to the mental health services offered by UCSF, the facility site is situated adjacent to mass transportation. San Francisco MUNI rail and bus transportation stops provide convenient transportation and access for patients and staff. A street-level coffee shop offers an amenity for family members, employees and the wider community to refuel or relax.
Outpatient space
There is a long history of people with psychiatric illness being marginalized. Poorly designed mental health facilities can signal shame and deepen feelings of stigmatization, resulting in people seeking care to forgo treatment. Matthew State, M.D., who serves as chair of the UCSF department of psychiatry and behavioral sciences, wanted a different outcome for the Nancy Friend Pritzker Psychiatry Building. The project goal was clear from the beginning: Whether a patient is 7 or 70, create a welcome, warm and safe experience that removes barriers to care.
The building location itself, sited on the edge of the UCSF Mission Bay Campus, enables patients to be fully part of the medical community rather than relegated to a faraway locale as is often the case with psychiatric facilities. Situated in the urban Dogpatch neighborhood, the exterior respects the unique look and feel of the San Francisco context with building massing and materials that complement the surrounding mix of commercial and residential uses.
Counter to other mental health facilities that are clearly marked as “other” with obscured facades or security protocols that can signal shame to patients entering the building, the Nancy Friend Pritzker Psychiatry Building provides lines of sight into the community and activity inside. Transparency and glass at the entry level emphasize openness to the community and normalization of the care happening within.
It is well established that first impressions of a space can influence the way a patient feels in a building, both physically and mentally, well beyond the initial visit. For the interior, the design team sought to harness the entrance moment by creating a gracious sequence that invites patients and visitors to a shared destination: the central atrium. Built-in safety and care control measures like separate entrances for children and adults allow the facility to provide a safe entry point while still offering a serene and visually connected environment.
The five-story, light-filled atrium acts as the heart of the building. Supporting goals for more transparency and openness, this center attraction is the nucleus with clinical, research and education functions flexing around it. The atrium provides the clear wayfinding and natural light, and contains the public-facing waiting rooms on all the floors, giving patients and families a sense of connection and belonging.
The vision for the interior design of the facility was to curate a warm and calming environment. The resulting palette is inspired by three distinct motifs: water, landscape and place. The San Francisco Bay and surrounding lakes are represented in public and connective areas to portray a sense of calm. Atrium openings evoke the curves of ships, making the space feel smooth and softening transitions. Environmental graphics on the atrium wall opposite the waiting areas visually tie to the atrium baffles and coils, emulating waves to provide a relaxing and engaging feature. Inspiration for the materials comes in part from San Francisco’s colorful “Painted Ladies” houses and the foggy ocean surroundings to evoke a comforting, humane environment.
Another distinguishing outcome of the goal to provide a welcome and warm experience is the rooftop healing garden. The garden boasts visibility to downtown San Francisco and the surrounding Bay Area. It is leveraged for staff to perform individual and group patient therapies. Staff also have a designated area for respite, outdoor dining and employee gatherings.
The facility’s approach to safety is tied to destigmatizing mental health care. UCSF wanted patients visiting for their basic care to feel like they were in any other standard health care setting. Key to ensuring safety for building occupants is the staff visibility to the entrances, circulation zones and waiting areas, along with staff engagements in the various open areas. There are three concentric security zones within the facility. The atrium is central to creating this sense of openness and transparency for the public, while providing safety via visual connectedness and a 6-foot-high glass guardrail at the atrium openings. The patient care areas are located via controlled access in the second zone, while access to the periphery is limited to researchers, faculty and staff only.
Research spaces
The facility design leverages integration of clinical and research for a multidisciplinary approach. Recognizing that psychiatry and psychology have a direct connection to neuroscience, the co-location is intended to advance the prevention and treatment of mental illness. By removing the traditional boundaries and silos that have historically existed between these disciplines and research studies within mental health care, the facility can assist clinical researchers in identifying precise diagnoses while also establishing effective treatment interventions more holistically and across a patient’s lifetime.
Multiple UCSF departments, including psychiatry and behavioral sciences, neurology, pediatrics, neurosurgery, obstetrics and gynecology, radiology and anesthesiology, will all have faculty in the building. In addition, a wide range of research resources are available, including for neuromodulation, neuroimaging, sleep, psychedelics, digital psychiatry and psychophysiology.
Highlighting the importance of research in the advancement of care, the psychiatry research spaces are not hidden within the building but integrated horizontally and vertically within the architecture. The placement of dry research space is accommodated throughout to support a variety of care across all age populations for current patient populations and for the future.
Situated adjacent to the child, teen and family center entrance, the neuroscape research space focuses on the latest psychedelic and neuroscience research. The translational neuroscience research program is dedicated to breakthrough psychiatry, neurology and neuroscience discoveries, and leverages interactive media, including virtual reality, for both assessment and treatment. The neuroscape room is an open space for sharing visual technology advances and discoveries but can also be closed off to allow privacy during patient treatments.
Identical room configurations allow for seamless transitions between patient care rooms utilized as a consultation room and dry research space including the utility requirements. During workshops, stakeholders evaluated room configuration via cardboard mockups to simulate room function and determine door and interior privacy glazing placement along with the furniture and utility needs. This standardization accommodated core clinical dry lab research space for neuromodulation programs, digital psychiatry and psychophysiology.
Transforming care
The Nancy Friend Pritzker Psychiatry Building seeks to radically transform the clinical care setting; enhance patient care, training and research; and offer a unique and powerful array of mental and physical health services for patients.
It is one of very few buildings in the country to bring together such a broad range of disciplines and capabilities for patients of all ages and is critically important in a time when the U.S. is facing unprecedented care gaps and ongoing stigma associated with mental health treatment.
The project will not only significantly increase access to mental health care for the Bay Area, it also intends to be a model for others to follow.
Solvei Neiger, AIA, ACHA, is a partner and health care practice leader at ZGF Architects. She can be reached at solvei.neiger@zgf.com.
Bringing diverse teams together to design for co-location projects
User engagement has long been a hallmark of the design process — bringing in diverse voices to provide valuable input and feedback, and ultimately to shape the design of each new project so it reflects the communities it serves. For the Nancy Friend Pritzker Psychiatry Building at the University of California San Francisco (UCSF), which incorporates the co-location of 20 clinical and research programs with varying approaches and needs, design workshops were critical for both initial buy-in and championing the eventual program results.
Regardless of the project and program, the following key elements for successful engagement with diverse groups can help to ensure success:
- Establish a clear project vision, guiding principles and rules for engagement at the outset. Remind stakeholders of these elements throughout the process. The practice of working together to create the vision and guiding principles will encourage everyone to participate, share ideas, ask questions and speak up, but also to have fun.
- Ensure program stakeholders or representatives are present for all meetings for continuity throughout the design process. These stakeholders are often a sole or one of a few representatives for their program and play a key role in relaying discussions to their teams.
- Clearly state meeting goals and objectives at the beginning of the meeting. Begin and end meetings on time. It is okay to set aside items for future discussions.
- Assign a mix of representatives to each team for design exercises. This allows for a necessary cross-section of voices and experts to explore and evaluate ideas. At UCSF, this led to one of the project’s most significant outcomes: the identification of program synergies and adjacencies, resulting in an integrated clinical and research model as well as the program building stacking by age from youngest to oldest.
- Remember that physical interaction is as critical as dialogue. When assessing design ideas, stakeholders should perform work with guidance and input from the design team resulting in user buy-in to the design approach.
- Use change management champions for a successful transition. Design- or program-focused user events are helpful for bringing siloed functions together to achieve a unified project goal, but they should always be paired with operational support from the health care organization. An internal resource who understands the organization’s real-life constraints around scheduling and operations is essential to bringing goals to life in any new space.