Exploring the world of architecture and bioethics

Health care facilities such as this suburban hospital are akin to medical interventions, and they require the same research depth and overview as pharmaceuticals or other therapies.
Image courtesy of WJH Health
Johann Goethe, the 18th century polymath, once remarked, “Architecture is frozen music,” by which he meant architecture interprets and expresses the values of its time — sometimes in a general epoch and sometimes at a very precise point. Experienced health care architects will appreciate this phenomenon, as current project drivers may have eclipsed those of decades past. It is in precisely this context that designers are studying the decisions and trade-offs that result from these normative preferences.
In health care architecture, design is being increasingly employed to affect patient outcomes, alter specific behaviors and mediate the interactions of those within health care spaces. The advances in design science have progressed to the point that the built environment in health care can be considered akin to medical interventions. And, as with medical interventions, the nature, risks, benefits and alternatives should be disclosed to patients and caregivers.
The ethics of buildings and construction typically involve environmental impacts and social equity of the built environment. And while these are important, the focus of this article is on the health care setting itself and how it affects patients, families and health care teams. While some of these effects bear on individual patients, such that an informed consent process may be sufficient, others have a population-level impact that will persist for generations, well after the designer’s direct influence.
Focused work in medicine, neuroscience and psychology is being employed to several ends but, to date, there has been little investigation of these practices. This is because the elements affecting control are neither providers nor medications, but the health care facility building itself. Broadly, this raises issues about the nature of the built environment, what constitutes a medical intervention, what architecture is expected to do and, importantly, what obligations emerge from designers’ choices.
To preview the impact of this argument, many facilities directors and design firms have built strong reputations in the architecture’s “ability to heal.” However, the truth and power of that proposition remain largely unexplored opportunities. While medical care itself forms the lion’s share of the healing enterprise, environmental factors can enhance or detract from those effects. Taking seriously the moral obligation to be knowledgeable and intentional about the powerful effects of the built environment in health care would enable architects and facility directors to validate such claims in the same way medical therapies are validated.
State of research
One consistent theme in the following examples is the demonstrable need for more research into the effects of these interventions, some of which are described below. Consider that roughly 5,000 articles in the Center for Health Design’s Knowledge Repository serve as the foundation that informs health care architecture. Compare that number to the 30 million peer-reviewed articles in PubMed that serve as the foundation of medical care. And yet, architecture has been linked to myriad physical, psychological and social effects, many of them in the health care setting.
The profession of architecture lacks the machinery that medicine or bioethics can call on for longer-term, project-spanning research enterprises. Therefore, evidence-based design requires a multidisciplinary approach involving changes at each level — at the bedside, in the project team room and in the executive suite. Some examples include:
- Design interventions coupled with health outcomes. Several significant examples of the utility of some research-informed architectural interventions include intensive care unit (ICU) room visibility, treatment intensity, patient falls, infection control and the perpetual debate related to centralized versus decentralized nurses stations. Nowhere is the need for more research more apparent than architecture being used intentionally to affect outcomes.
Roger Ulrich’s pivotal but small 1984 retrospective study examined hospital stays in postoperative patients in which one group’s hospital window faced a brick wall and the other faced a park. The group facing the park had shorter hospital stays and took fewer doses of pain medications. This study launched the field of evidence-based design, as architects claimed professional validation by evidence to support what they had instinctively believed. In the ensuing decades, many studies examined nature’s role, with findings supporting the hypothesis that access to nature and views of nature reduced stress, lowered blood pressure and diminished the need for pain medication.
Other research has found that facility design can affect the care choices made by physicians and medical teams. A Harvard lab investigated different rates of caesarian sections that correlated with elements of the building’s design. A small number of labor and delivery suites and a larger number of surgical recovery bays prompted providers to move from natural birth to surgery more quickly than in other facilities. In effect, the building plan profoundly affected the care that went on inside it.
- Nudging and illusion for cognitive impairments. The bioethical connection between architecture and dementia is neurological; for example, the brain regions affected in the early stages of Alzheimer’s overlap with the areas important for spatial navigation. Research into these impacts has revealed perceptual disabilities in persons with dementia (PWD) that in certain settings may limit the navigation of PWD while not affecting others. Instead of managing the disruptive behaviors through traditional methods (e.g., locking exterior doors, physical restraint or the use of medications), design-based approaches may utilize these perceptual differences of PWD to decrease disruptive behaviors.
For example, PWD often avoid shiny floors and surfaces with extreme glare, grid patterns on floors and black areas on floors. Even though these design interventions do not slow or halt the progression of dementia, they are effective at decreasing the use of traditional methods of behavior management in PWD, such as chemical or physical restraint.
Across the world, dementia facilities are increasingly employing design-based approaches to similar effects. However, these interventions rely on creating a misperception of the space. The natural progression of this illusory approach is complete immersion. For example, De Hogeweyk, the original “Dementia Village” set in the Netherlands, does not limit resident wandering but promotes permissive wandering to combat the confusion and spatial disorientation experienced by PWD through a created reality. In the Dementia Village, residents are free to visit amenities such as shops, a café and a pub; and purchases are made with fake money, lending a sense of realism to transactions.
Anecdotal reports from De Hogeweyk note less agitation and behavioral disturbances in addition to fewer doses of psychotropic medications, although no formal studies to date have attempted to quantify the village design on outcomes, nor have those outcomes been defined. Is the absence of medications or restraints alone the correct metric, or should any effects on a resident’s primary health and well-being also be considered? Do these interventions temporize the behavioral symptoms of dementia or even other unknown consequences?
- Using design to segregate patients and staff. Health care facilities typically separate staff, patients and families. For example, private patient rooms are special spaces that allow for critical communication under controlled conditions. However, the practice of medicine is actively moving toward improved transparency and promotion of patient autonomy, diverging from the traditional architecture of hospitals, which often reinforces a clinical process that remains opaque to patients.
Recent design approaches borrowed from the hospitality industry to deliberately segregate staff activities from patient- and public-facing activities. While the intent is to improve patient satisfaction (a managerial metric), staff often become isolated from the spatial benefits otherwise afforded to patients. This trend is likely to intensify in the coming years, as contagion considerations add weight and volume to calls for separate spaces in a post-COVID-19 world looking to avoid another pandemic. Additionally, staff caregivers are already demanding better working conditions to support work-life balance (see Figure 1 below).
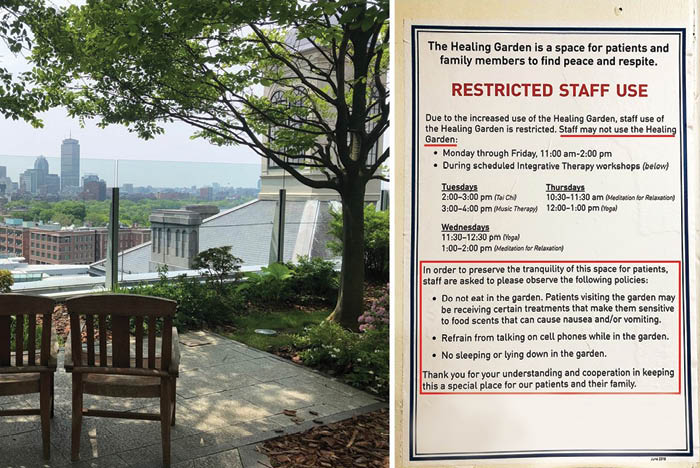
Figure 1: Staff are prohibited from accessing a hospital garden amenity to be used for public only, resulting in space that is often unoccupied.
Image courtesy of WJH Health
Physician burnout and moral distress have been linked to poorly designed workflows and systems, which include chaotic environments, interruptions and distractions. Frequently, the hospital lobby, waiting areas and public eating zones are enhanced with art, color and amenities. But, as one crosses the consumer-design threshold into the off-stage portions of the building, the walls often become colorless, lighting becomes harsh and views of the outdoors are reduced. The resulting fragmentation, decentralization and concealment of clinical spaces create class disparities between staff and patients, a condition at odds with the current social discussions around equity and a stressor to human resource directors filling and retaining staff roles.
Ramifications for architects
If one accepts the basic notion that health care architecture is itself a medical intervention — as is often claimed by many designers and researchers — the responsibilities of their effects carry direct ethical obligations.
This is completely new territory, and many design firm attorneys will immediately claim that the standard of care is being extended. However, a high standard already exists in the research demonstrating generalizable or even specific effects. All involved in design do not have the luxury of being complacent, but these realities already demonstrate a higher order of knowledge, practice and even outcomes.
Similarly, all health care enterprises accumulate enormous amounts of data through their own internal research initiatives. As a matter of the design process, architects should be asking for specific data to develop metrics and demonstrate the value of their work in clinical efficacy, operational benefit and outcomes. The implied value proposition is significant and allows for a deeper demonstration of cause and effects regarding better patient and community outcomes, which have the potential to reduce clinical and operational costs or even enhance value for health systems.
- Obligations to inform about architectural effects. With increasing knowledge of how architecture impacts patient well-being and outcomes comes the responsibility to be transparent about those effects. Health care organizations regularly conduct institutional and quality control surveillance to optimize various behaviors and policies known to affect outcomes; for example, the use of checklists to minimize surgical site infections, moving high-risk procedures to specialized services and promoting cultures of safety.
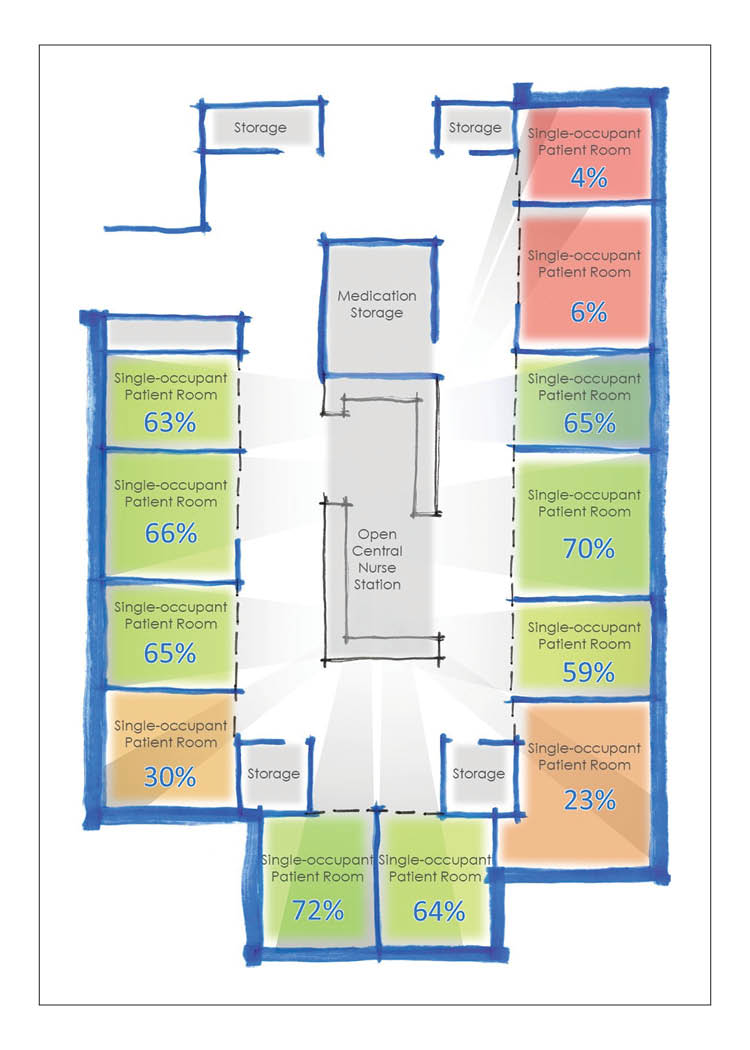
However, institutions less commonly perform design-based interventions to optimize outcomes. While the impact of behavior has a role to play, physical design is often overlooked as one of the most powerful motivators of behavior, as an ICU study examining patients placed in rooms with poor nursing visibility demonstrates (see Figure 2 to the right).
Because designers know the built environment has profound effects on those within a space, and designers have a duty of care to its occupants, all of those involved in making decisions with this knowledge must not just be transparent about those effects but also be intentional about how one uses that power. If there are concerns that poorly visualized ICU rooms tend toward poorer outcomes, those in the architectural, medical, bioethical and public health professions should address the benefits and harms of differing designs directly.
Design and health care teams should work to maximize both outcomes and fairness to all patients, regardless of which ICU room those patients find themselves in. This has a current corollary with how health facility risks are assessed with an infection control risk assessment or a disaster, emergency and vulnerability assessment, or even more deliberate oversight that is required in the development of pharmaceutical trials. Whether the cause of the disparity or potential harm to patients is the building itself or a medical treatment, it should be addressed during design.
- Weighing the benefits and harms. The harms and benefits of different design options depend on one’s perspective. Some argue that creating artificial realities such as dementia villages is an affront to their dignity. Others argue the benefits of design-based interventions, which diminish disruptive behaviors by using such illusion and deception, are justified by limiting stress, conflicts with staff and the indignities of being sedated.
The potential for harm in traditional dementia care facilities that employ physical restraint and sedation might further outweigh the harms of the illusion and deception. On the other hand, the means of these interventions are at odds with principles of respect for individual autonomy and truth-telling. In the end, careful consideration of these issues and deliberate decision-making by all stakeholders is a high road forward into this unexplored terrain.
Architects are ideally suited to take a leadership role in the advancement and selection of these techniques. However, to be leaders in this new space, architects will not only need to collaborate with the physicians, bioethicists and scientists doing this research but also become versant in the ethical questions and issues that emerge.
By synthesizing the research and value considerations, architects are ideally positioned to assert a new level of professional authority beyond being an educator exclusively into a professional domain that may extend beyond health, and which pushes the envelope of how the built environment can improve the human condition.
Expanding the discussion
A way forward may recognize that health care environments are what Donald Berwick recently described as a “moral determinant of health.” The researching, designing and construction of these environments can have as much impact as the best therapeutic intervention or the worst ethical breach of a patient’s rights.
All involved with health care design need to preserve and assist all stakeholders’ abilities to act intentionally or make deliberate choices about relinquishing freedoms. The issues raised here are distinctly architectural and bioethical, and they actively invite discussions about these issues with project teams, hospital-based ethicists, institutional review boards and executive leaders.
The value proposition offered is substantial for the future of health care design in general, and for architects to engender and assert professional authority. This may be done through responsible consideration of applied research, engaging with concurrent research studies conducted within their client’s domains, and advocating for longitudinal research related to sustained outcomes.
Basic recommendations on interventional hospital design
The health care built environment should in many cases be considered a medical intervention, and it should therefore be subject to the same research depth and overview as medical interventions.
This is especially true when design elements utilize knowledge of cognitive impairments to influence behavior, associate with relevant medical outcomes, and become a source of burnout or inequity for staff.
While this work just begins to discover the full scope, impact and ethics of the built environment as a medical intervention, several basic recommendations can be drawn:
- The development of architectural interventions intended or known to have effects on patients compared to other medical interventions should be rigorously reviewed.
- The question of design standard of care should be openly and honestly discussed, recognizing the legal implications and potential increased value of design services.
- Informed consent should disclose any design interventions aimed at modifying behavior, whether as part of the hospital admission process or when moving to a long-term care facility.
- Surrogate consent to long-term care involving deception or illusion, particularly when against the patient’s wishes, should be subject to additional oversight and scrutiny.
- Hospital quality improvement departments may consider monitoring the effects of their built environment on relevant patient outcomes and examine more architectural interventions to improve outcomes.
- Health care institutions should strive for spatial quality parity; high-value spaces are community assets that can build a sense of comradery, solidarity and trust between staff, patients and their families.
- Health environments research needs suitable and substantially more funding to create a credible research infrastructure to demonstrate clear cause-and-effect relationships, akin to those afforded medicine or other therapies.
- Organizations could reconsider contractual relationships to include longitudinal data collection and research.
William J. Hercules, M.Arch, FAIA, FACHA, FACHE, is an architect and the CEO of WJH Health; Diana C. Anderson, M.D., M.Arch, ACHA, is a health care architect and physician who is a principal at Jacobs and a clinical fellow at the VA Boston Medical Center; Stowe Locke Teti, HEC-C, is a clinical ethicist with Inova Health System who teaches ethics to Georgetown University and University of Virginia medical students and is editor-in-chief of the bioethics journal Pediatric Ethicscope; and David A. Deemer, M.D., MA, is a bioethicist and internal medicine resident at the University of Wisconsin. They can be reached at Bill@WJH-Health.com, diana.anderson@dochitect.com, stowe.teti@inova.org and ddeemer@wisc.edu.