Mitigating climate threats through diligent planning

The Kaiser Permanente Lutherville-Timonium Medical Center in Timonium, Md., has a 450-kilowatt solar array on the roof of an adjacent parking garage that supplies 18% of the power to the building, greatly reducing its greenhouse gas emissions and providing resiliency against a grid outage.
Image by Chad Baumer and facility design by Gresham Smith
The effects of climate change are the foremost contributors to the steadily increasing cost of extreme weather events throughout the United States
According to the National Oceanic and Atmospheric Administration (NOAA), the average annual cost of billion-dollar weather and climate disasters in the U.S. has risen from approximately $6 billion in the 1980s to nearly $50 billion in the 2010s. In 2022, the U.S. experienced 18 separate weather or climate disasters that each resulted in at least $1 billion in damages.
The financial impact of extreme weather events can be felt in many ways, including lost income, increased health care costs, damaged infrastructure, and increased food and fuel prices. These costs can also have a long-lasting impact on communities, particularly in low-income areas where physical and economic recovery is difficult.
Overall, the cost of extreme weather events in the U.S. highlights the importance of addressing climate change and investing in measures to mitigate its impacts and reduce the risks it poses to communities across the country.
Protecting populations
Projections show an increase in the frequency and intensity of extreme weather events, such as hurricanes, floods and heat waves, which can disrupt health care services and cause widespread damage to health care facilities and infrastructure.
Health care systems play a critical role in protecting public health and are often at the forefront of the response effort to the increasing frequency of extreme weather events. It is essential that they continue to function during and after extreme weather events.
Additionally, climate change can exacerbate existing health disparities of economically disadvantaged populations. Because health care systems bear responsibility to address these social and environmental determinants of health, planning for resiliency will help them prepare for these challenges.
A diverse range of stakeholders, including health care professionals, climate experts, policymakers and civil society organizations, have come together to collaborate and coordinate their efforts to address the health impacts of climate change. This includes strengthening health systems to respond to the impacts of climate change and increasing awareness and understanding of the linkages between climate change and poor health outcomes. As Michael Boninger, M.D., of the University of Pittsburgh Medical Center (UPMC) puts it, “[The] health care [field] can’t cause the diseases we are trying to treat, and [we] must take action to reduce our own greenhouse gas emissions.”
Rallied by its internal Clinicians for Climate Change group, and with support from executive leadership, UPMC made the commitment to a more sustainable future in 2022. In the short time since then, UPMC has formed its Sustainability Center with a multidisciplined team dedicated to reducing greenhouse gas emissions, improving the efficiency of its buildings, making sustainable purchasing decisions and expanding the resiliency of its organization. The intent is to show these goals can be achieved in a fiscally responsible way that shows UPMC’s dedication to its employees, patients and the community as a whole.
Resources
Kaiser Permanente, Oakland, Calif., long known for its commitment to sustainability and resiliency, understands that where people live and work profoundly impacts their health. “When we evaluate sustainability and resiliency strategies, we look at not only what it means in terms of our own organization, but the important role Kaiser Permanente has as a leader on environmental stewardship,” says Seema Wadhwa, executive director of environment stewardship. Kaiser Permanente has been on its sustainability journey for many years and was the first health care system to be certified carbon neutral in 2020.
While Kaiser Permanente had emergency management plans related to climate change in place for many years, the health system appreciates that there is now a focus on this for the health sector and that many health systems are recognizing the importance of being prepared for the inevitability of extreme events in the future. This was never truer than when Kaiser Permanente had to put its emergency response plans into action in 2017 and 2019, and staff twice evacuated its Santa Rosa Medical Center due to encroaching wildfires. Thanks to well-established emergency response plans, Kaiser Permanente was able to safely evacuate more than 120 patients and ensure continuity of care.
With the advent of many health care systems committing to sustainable and resilient organizational goals, architects and engineers must become good stewards of the execution of these promises. They need to play a critical role in helping health care systems meet their commitments and be more resilient in the face of extreme weather events and other climate-related health threats.
Designing for resiliency
Architects can design health care facilities and infrastructure to be more resilient, incorporating features such as redundant mechanical systems, backup power generation and elevated structures that house these systems in areas prone to flooding. Ensuring that systems and structures have multiple layers of protection and that there are multiple access pathways for essential services to reach the community is critical.

Design thinking sessions can be used to identify issues and creatively solve problems.
Image by Getty Images
It is important that architects design systems and structures that can quickly and easily adapt to changing conditions, such as shifting energy sources, changing demographics or changing economic conditions. Encouraging community involvement and participation in the planning and design process ensures that the design reflects the needs and priorities of the community.
Planning and designing for the long term while considering the probable impacts of climate change, resource depletion and other challenges is key to success. Considering the interconnections and interdependencies between different systems and structures, such as transportation, energy, water and waste management, and designing them in a holistic and integrated manner will culminate in optimal resilience.
Climate risk assessments
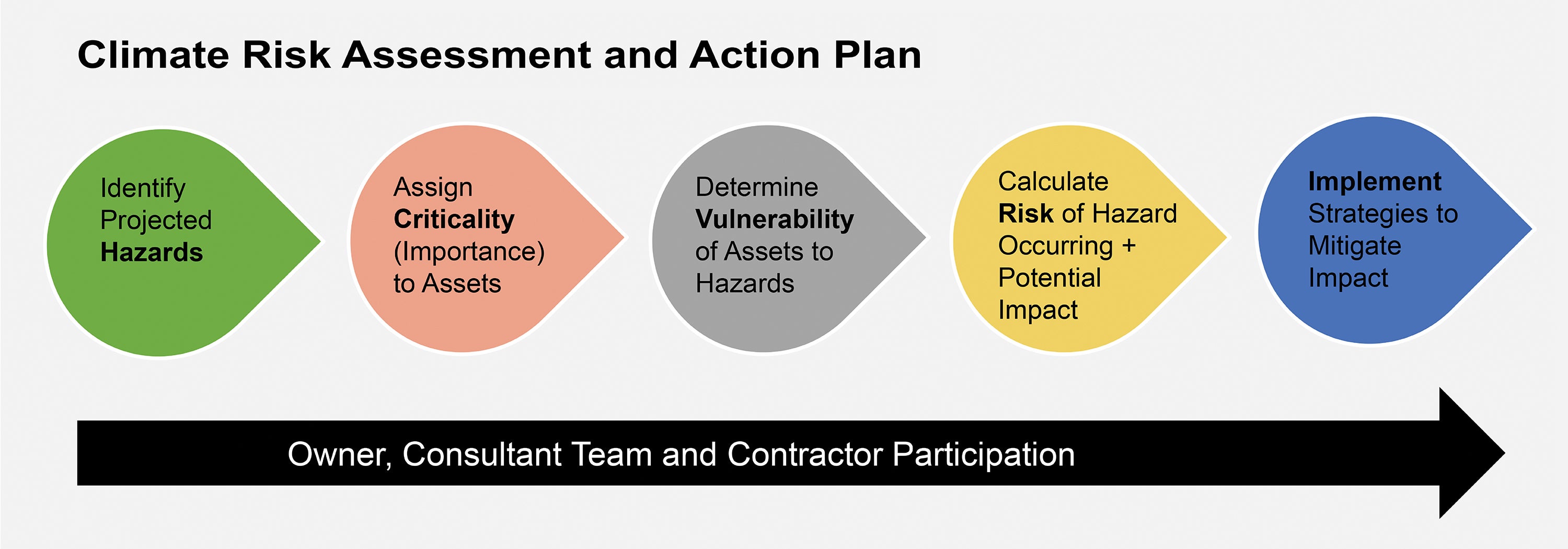
A climate risk assessment evaluates the potential impacts of current and future climate change disruptors and analyzes the vulnerabilities of an organization’s assets and systems to these disruptors. It is based on the best available data and considers local conditions and priorities.
The goal of a climate risk assessment is to identify the potential risks and prioritize actions to mitigate or adapt to those risks. This allows an organization to reduce the likelihood and severity of negative impacts and maintain business continuity. For health care organizations, this means the ability to continue to care for patients before, during and after major events. A climate risk assessment involves four steps:
- Identify the project hazards that might be a threat to the organization or the region over the next 75 to 100 years. This can be accomplished using tools such as the U.S. Climate Resilience Toolkit and specifically the Climate Mapping for Resilience and Adaptation software.
- Determine the importance of each asset or operation of the organization to the overall business continuity and assign it a criticality.
For example, these assets might include people, operations, buildings, inventory, data and equipment. An asset might have a low criticality if its loss or interruption would have a negligible impact on the function of the organization, a medium criticality if its loss would hamper the function of the organization, and a high criticality if its loss would significantly impair or shut down the organization until repair or replacement was completed.
- Determine the vulnerability of the assets to the hazards by identifying the assets exposed to the climate hazard and determining the sensitivity and the adaptive capacity of each asset to each hazard.
- Calculate the risk of the hazard that’s occurring and the potential impact on the organization if it does occur or the magnitude of the loss should it occur.
Climate action plans
Once a climate risk assessment is complete, a climate action plan is developed to outline how an organization will implement strategies to mitigate the impact of major events. The plan typically includes a series of specific, quantifiable goals and targets for reducing consumption and, therefore, emissions, such as increasing renewable energy use, improving energy efficiency, reducing potable water use and reducing waste.
It also includes strategies for building resilience to the impacts of climate change. This includes improving infrastructure to better withstand extreme weather events, preserving ecosystems that provide natural protection from storms and flooding, and investing in research and development of innovative technologies. Strategies for resilience include:
Building hardening. Building hardening can mean different things based on the building’s location and the potential threats it is likely to face in the future. In areas prone to flooding, this means ensuring the finished floor elevation is above a certain flood level. In areas where hurricanes are prevalent, it means designing a structure and envelope system that can withstand very high winds. In areas where the heat index continues to rise, it means incorporating additional cooling capacity and, in areas where wildfires are a threat, it means ensuring a robust indoor air quality and filtering system.
Improving energy efficiency and backup power. Architects and their engineering partners can design health care facilities to be energy-efficient, reducing their overall environmental footprint and their dependence on fossil fuels. By reducing the amount of energy needed to perform tasks, the dependence on external energy sources, which can be interrupted in a major event, can be reduced.
Additionally, reducing the amount of energy to run the building will make emergency sources of energy last longer when the grid is interrupted and normal energy sources are unavailable. Providing a redundant feed to and from the electrical grid and extra capacity in the building’s mechanical system will also increase a building’s resiliency.
Energy efficiency also can lead to lower energy bills, which can help reduce the financial burden on health care systems, making them more resilient in the face of economic challenges. All these energy efficiency strategies work together to help reduce greenhouse gas emissions, therefore accomplishing a reduction in emissions while prolonging backup capacity.
Increasing the use of renewable energy sources. Renewable energy can provide energy security by reducing the dependency on the electrical grid, making organizations less susceptible to interruptions from power outages. These may include solar, wind or thermal-sourced equipment. Once installed, renewable energy systems are typically less costly to operate and maintain. Additionally, these power sources emit little to no greenhouse gases, which can help reduce the impacts of climate change.
Reducing potable water use and identifying alternate sources. Just like energy efficiency, potable water use reduction helps address environmental concerns, such as water scarcity and ecosystem protection, but also reduces an organization’s dependence on water that is typically a municipal-provided utility.
By reducing the total amount of water needed to operate the health care facility, the secondary source of potable water that might be needed in an emergency is also reduced. Alternate sources of water are essential to a resiliency strategy and can include in-ground wells, rainwater collection and grey-water reuse.
Reducing waste. Reducing waste can contribute to reducing greenhouse gas emissions by limiting the energy needed to produce new goods, reducing the emissions from the transportation of waste and reducing the amount of methane produced in landfills. Architects can design with long-lasting, durable materials to avoid replacement costs.
The selection of materials should be carefully considered to provide the best life cycle cost to the owner. Waste reduction encourages a shift toward more sustainable production and consumption patterns. This can lead to more certainty in supply chains, which are robust, adaptable and better equipped to handle supply disruptions and uncertainties.
Incorporating green spaces. Architects can incorporate green spaces, such as parks, gardens and green roofs, into the design of health care facilities, promoting public health and helping to mitigate the urban heat island effect. Green spaces can:

The courtyards and green roofs at the UF Health North Campus in Jacksonville, Fla., help reduce the heat island effect of the campus and control stormwater runoff while also providing opportunities for patients and staff to decompress and connect with nature.
Image by Ryan Ketterman and facility design by Gresham Smith
- Help absorb rainwater and reduce the risk of flooding, resulting in health care campuses becoming more resilient in the face of extreme weather events.
- Provide shade, cool the air and reduce the urban heat island effect, providing human comfort in the face of increasing heat waves.
- Absorb carbon dioxide and pollutants and release oxygen, improving air quality and helping to reduce the risk of respiratory distress and other health problems.
- Provide habitat, which also results in making communities more biodiverse in the face of these ongoing environmental challenges.
- Reduce stress, improve mood and increase overall mental well-being, helping communities respond more positively in the face of social and psychological challenges.
- Provide opportunities for outdoor recreation and physical activity, helping to improve public health and reduce the risk of chronic diseases, and allowing communities to encourage healthy behavior to mitigate increasing health challenges.
Improving transportation access. Understanding the transportation routes for supplies, aid workers and food is essential to a resiliency plan. If these routes are likely to be interrupted in an emergency, it is important to have a plan to stockpile the items that might be needed during the emergency.
Stakeholder collaboration
Architects should work closely with health care providers, public health officials and community leaders to understand the specific needs and challenges faced by health care systems in their communities and to collaboratively develop solutions that promote resilience and positive public health outcomes.
Ultimately, designing for resilience involves considering a range of factors to create systems, structures and communities that can withstand and quickly recover from disruptions, thus increasing overall resilience and reducing vulnerability to weather events.
About this article
This feature is one of a series of articles published by Health Facilities Management in partnership with the American College of Healthcare Architects.
Julie Mullen, AIA, ACHA, LEED AP, is senior operations leader, and Corie Baker, AIA, EDAC, LEED AP BD+C, WELL AP, Fitwel Ambassador, is health care strategy leader for Florida at Gresham Smith. They can be reached at julie.mullen@greshamsmith.com and corie.baker@greshamsmith.com.