Now + forever
 When planning for new patient rooms, today's health facility professionals have quite the challenge. They must ensure that the room design will provide effective, state-of-the-art technology when the space is initially occupied and adapt to future technologies.
When planning for new patient rooms, today's health facility professionals have quite the challenge. They must ensure that the room design will provide effective, state-of-the-art technology when the space is initially occupied and adapt to future technologies.
This is easier said than done. Depending on the size of the project and funding, it may be years before the space is actually constructed and ready for occupancy. Working closely with a knowledgeable medical-equipment planner will increase the probability that the design will last well into the future.
Three types of rooms
Most hospitals have three general types of patient rooms, depending on the acuity level of the patient: intensive care unit (ICU) rooms, step-down or intermediate care rooms, and acute care rooms.
ICU rooms are grouped together in a unit to take advantage of the nursing skills required to care for these patients. These nursing units are called medical ICUs, surgical ICUs, cardiovascular ICUs and cardiac ICUs, to name a few.
Each type of patient room must accommodate an extensive array of specialized medical equipment required to care for the clinical needs of the specific patient population. Consideration also must be given to the safe and efficient use of fixed and movable medical equipment brought in to care for the patient. They also must accommodate nursing staff and the cardiac resuscitation team, if they are needed. Consequently, these rooms need to be designed to allow safe, easy access to all sides of the patient.
Once the types of equipment that could be used in the room and the location and position of the patient are known, the room layout can begin.
Room organization
A major consideration for an ICU room is getting the utilities to all the movable and portable equipment brought in and out of the room during a patient's stay. The ceiling, wall and floor space are usually at a premium in these rooms and the anticipated use of specific medical equipment will dictate the location of both the fixed and mobile medical equipment.
Types of utilities and outlets that typically need to be available in the room range from electrical and emergency power receptacles for equipment (e.g., ventilators, hemodialysis units and physiologic monitors); to low-voltage connections for various devices (e.g., television, information technology data lines for bedside physiologic monitors, electronic medical records and alarm monitoring); and medical gases (e.g., oxygen and medical air and vacuum outlets).
There are several methods of getting the utilities near the patient. Fixed floor-to-ceiling columns and movable ceiling- or wall-mounted booms have been gaining popularity over a standard prefabricated headwall or mounting the utilities directly on the walls adjacent to the patient bed. The columns provide better organization of the devices, better accessibility for staff and reduced wire and tube clutter, and fewer tripping hazards.
The columns and booms also allow for some bed movement to take advantage of window vistas, which have been attributed to patient well-being. However, window views may not always be an option due to existing external obstructions. One innovative hospital solved that dilemma by planning to install windowlike frames to display real-time camera views from several locations on the hospital roof.
If a fixed column or boom is used, space on the ceiling needs to be evaluated for proper layout, ceiling support structure and lighting requirements. Some ICU rooms may be equipped with one or two special procedural lights mounted in the ceiling above the patient for procedures that could be performed in the room in an emergency. Procedure lights sometimes are specified for ICU rooms. One model enables lights to be directed to the specific site using a wand- or wall-mounted panel.
Another consideration competing for ceiling space is the patient lift. Patient lifts can be mounted to the ceiling, installed as freestanding structures, or attached to a boom. The Facility Guidelines Institute's 2010 Guidelines for Design and Construction of Health Care Facilities identifies the need to conduct a patient handling and movement assessment and to address this during the construction process, which could have major implications for room design.
If there is a possibility of installing ceiling-mounted lifts in the future it is prudent to plan for them in the early design stages to prevent clashes with structures above the ceiling or to add structural support while the room is being planned.
Nursing staff need good visibility to the patient from the hallway. This is accomplished by using a significant amount of glass. However, sometimes privacy is needed for the patient and switchable or so-called "smart" glass is used in some units to accommodate the dual needs of privacy and observation.
With the touch of a switch, the glass changes from transparent to opaque, blocking light and providing privacy and security. This high-tech glass eliminates the need for blinds or curtains that may present an infection control risk and pose a cleaning challenge for environmental services. These glass panels are relatively expensive compared with that of standard glass, however.
Equipment needs
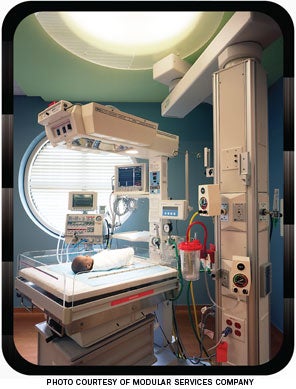 |
| This is Modular Services Company's equipment solution for neonatal intensive care operations. |
The design team must ensure that the room is future-proofed for all of the equipment that may be fixed or wheeled into the room. It needs to consider the possible uses of the room when it is completed as well as how the room may be used in the future.
Ultimately, the type of critical care unit and patient determines which technologies are needed in the room. Most ICU rooms include ventilators; physiologic monitors mounted on a wall, boom or column; IV poles that are movable or mounted to a column or boom that can accommodate multiple IV pumps; and patient-controlled analgesia pumps. All of these may require multiple emergency-power receptacles.
Many of these devices will be integrated with the hospital electronic records through wireless connections. This integration requires that the information technology (IT) group be intimately involved with the planning of the room design and antenna placement.
Some facilities monitor ICU patients from a remote site, often called the electronic ICU or command center. For remote-monitored rooms, a pan-tilt-zoom (PTZ) camera, microphone and speakers — either ceiling- or wall-mounted — are needed to enable the remote site to communicate with the patient or nursing staff and observe patient and vital equipment displays and settings.
There is also a telepresence robot on the market that can be maneuvered into the room to gather the same type of information. This type of device requires a clear floor path through the room without wires, tubes or cables on the floor.
Intelligent patient beds are another new component in high-tech patient rooms. They not only require electrical power, but also a low-voltage data jack to connect to the hospital infrastructure for nurse-call and bed-exit alarms to monitor for fall risks. They also require connections for electronic medical records.
The flow of patient care within the room needs to be planned carefully to accommodate wireless workstations on wheels (WOWs), which typically are used for patient charting and confirmation of medication delivery. While they do not require an electrical receptacle or data jack, they take up space and need to be considered in the room layout. The typical footprint for the WOW is approximately 26 inches wide by 28 inches deep; however, newer tablet devices eventually may supersede WOWs for charting patient care.
As more and more new technology is introduced for patient care, the design team faces new challenges in providing the required utilities and adequate footprint. For example, ICU patients too ill to be moved for imaging studies need space in their rooms to accommodate mobile imaging devices like a mobile C-arm radiography or fluoroscopy unit.
The type of patient receiving care will dictate the equipment and utility requirements for the room. Here are some examples of typical ICU room equipment that have relatively large footprints and their utility requirements:
- Hemodialysis equipment using continuous renal replacement therapy requires a hot and cold mixed water supply, drain and emergency power.
- Ventilators require emergency electrical power, a medical air connection and a data connection for alarm management.
- Hypo/hyperthermia units require electrical power.
- Intra-aortic balloon pumps used in the cardiovascular ICU require emergency electrical power.
- Video endoscopy carts or bronchoscopy carts require electrical power.
- C-arms require electrical power.
Space also is required to ensure quick patient access by the resuscitation team with their resuscitation cart or crash cart.
Other types of ICU rooms may require very different equipment needs. For example, specialized orthopedic beds in a trauma ICU that provides for traction are usually larger and have bars that extend toward the ceiling. These require clear space above the bed to accommodate the bars. Likewise, neurologic intensive care areas may call for specialized monitoring equipment that require data jacks as well as a ceiling- or wall-mounted PTZ camera and microphone and speakers.
Point-of-care technology may have an impact on additional requirements for the design of the room as blood gas monitoring and portable ultrasound are becoming more prevalent. The key is using the medical-equipment planner to provide those glimpses into the technologies of the future of patient care and to raise the awareness of potential implications of the design on future needs.
Decisions must be made about making the investment to provide for the necessary flexibility, or at least addressing the potential impact, and designing the room to be able to add future equipment or technologies.
Beyond the ICU
Critical care areas aren't the only sections of hospitals with high-tech patient rooms. Step-down rooms and acute care rooms have their share of technologies requiring planning and installation considerations.
Step-down rooms are associated with the ICUs and have a reduced complement of equipment needs depending on the type of step-down unit. These rooms may be monitored via a telemetry transmitter that sends a patient's heart trace signals and maybe pulse oximetry to a central monitor that is being watched by a trained monitor technician. A step-down room also has a lesser requirement for both the regular and emergency electrical power systems and the number of oxygen, medical air and vacuum outlets. The design may have to accommodate fixed-ceiling patient lifts.
The acute care room has an even smaller complement of medical equipment and, consequently, less infrastructure. Some health care facilities are designing step-down and acute care rooms to be more like hotel rooms, conveying a less clinical and more comforting experience for both patients and their visiting family and friends.
Many hospitals also treat critically ill infants and children. Neonatal and pediatric ICUs have highly specialized equipment and unique room design requirements.
More of these rooms are being designed as private rooms to provide better control over the sensory environment for the neonate. Alarm management from the equipment in the room requires data jacks. Lines of site that are lost due to privacy and communication challenges need to be addressed with technology because of hard walls. Equipment to care for the neonate can be mounted on the wall or suspended from the ceiling on a boom. Utilities like regular and emergency electrical power are needed in sufficient quantity. Additionally, medical air, oxygen and vacuum are required, as are data jacks for connection to the central monitoring and the hospital information systems.
Planning for future
While considering the equipment now used in each type of room, hospital designers and facility managers must work in conjunction with clinicians to consider the potential use of the room in the future.
It is generally easier and less expensive to include additional space, electrical and data outlets, and utilities while in the design and construction phase of a project, rather than waiting until the spaces are occupied with patients and then deciding an upgrade is needed.
John J. Skreenock, HEM, is senior associate for the Applied Solutions Group at ECRI Institute, Plymouth Meeting, Pa. He can be reached at jskreenock@ecri.org.
| Sidebar - Flexible rooms provide savings |
| A medium-sized hospital planned to renovate a couple of its acute- care nursing floors and convert all of the semiprivate rooms to private rooms, creating a new intensive care unit (ICU) step-down space. While initial plans called for the rooms to be used for step-down patients, the longer range plan was to convert these spaces to ICU rooms when needed. For a step-down room, telemetry monitoring is sufficient. However, for future use as an ICU setting, centrally monitored, wall-mounted physiologic monitors or other high-technology equipment would be required. With that in mind, the design had to be modified. The hospital decided to plan the rooms with increased infrastructure to handle the future conversion. Increased gas and vacuum capacity for additional outlets and additional electrical power and data jacks allowed for future upgrades. These design changes now allow the high-technology equipment that is routinely deployed in the ICU to be used in these rooms in the future. The cost for such infrastructure at such an early stage is a fraction of the cost required in the future to convert the rooms. However, cost is only one factor that would be considered for future conversion. If the hospital had not increased the infrastructure during the original renovation, a future conversion would have faced major complications, including the potential loss of revenue while the rooms were being renovated extensively, disruption to patient care and department operations, complex infection-control issues and a longer time to complete the conversion. With all of these considerations, the conversion for ICU patients may never have happened. |
| Sidebar - Prepping for mass patient surges |
| When hospitals need extra space for unplanned patients in mass numbers, such as during or after a flu epidemic or a disaster with mass casualties, some facilities provide a flexible solution for allowing the census in a particular nursing department to flex up in times of need and then flex back down when the need subsides. A portion of the acute care private rooms are designed with the ability to accommodate two patients in the same room, essentially creating a semiprivate room. This flexibility is provided by having the room designed with built-in infrastructure, such as utilities to accommodate two beds. The design requires two headwall arrangements, each with enough gas and vacuum outlets; regular and emergency power; data jacks for plugging in equipment that communicates with the hospital's information systems; and separate lighting controls for each bed. Movable equipment required for patient care, like beds and IV pumps on poles, can be wheeled in when needed. The second bed can be set up similar to the first but may not need all the amenities, because it only would be used for a short duration. Flexibility designed into the rooms allows for an unexpected short uptick in the hospital census. The surge plan then will call for fixed medical equipment as well as additional mobile medical equipment to provide patient care. The mobile equipment may be relocated from another area of the facility, from storage or requisitioned from local rental firms. |




