Information flow
As the push to build more with less grows, the term "lean design" has taken on increased significance in the health care field. Owners and designers have begun to embrace streamlined technology planning for the increased efficiencies, improved quality of care and reduced costs it provides during the hospital construction or renovation process.
In the field of health care technology, lean design refers to reducing inefficiencies and minimizing risk; both of which translate into buying down cost risk. To achieve this, the designers of the system that supports medical and operational data must approach the process in a way that seems counterintuitive to conventional practice. But the payoff can be great.
A shift from the norm
The design and implementation of technology can be mystifying because of its complexity. It is evolving and changing constantly. Because of this, technology designers typically refuse to make firm commitments on systems until the construction phase of the project.
This makes those responsible for building-design coordination and budget nervous, because a huge piece is seen as up in the air until the latter part of design and construction.
The lean process requires a change to this way of thinking by advancing the design of the technology systems earlier in the process. This means committing to buy out certain products and bring on subcontractors as trade partners.
This approach typically is resisted because it may lead to building a hospital that is technologically obsolete when the doors open. Successful implementation of lean design must strike a balance between early design and technology obsolescence.
Is it possible to push the technology design up front and retain the ability to flex system choices as technology changes during the course of the design and construction of the project? Yes, though there are some drawbacks. Using the lean process can be successful and, in fact, preferable to the traditional late-stage design method for technology. The lean process pushes innovation in the quest to reduce inefficiencies.
The payoff? If done right, it makes one think about how the technology will enhance the operational flow of the facility. It is possible to commit to certain aspects of a plan and still leave options open for technology changes without negatively affecting design and budget.
Setting the stage
How the stage is set in the beginning determines the project's overall success. Those new to this approach to technology planning may question the benefit of shifting more detailed design up front.
Benefits are hard to pinpoint in the beginning, when it seems as though productivity is lost in exchange for considerable changes and rework. This concept is foreign to traditional design methods. After all, options usually must be researched and owner decisions made before design begins.
Here is where one must change the paradigm. The technology designer's role is to take control of the process and push the research and consequential decisions up earlier in the process. This is the cornerstone of a successful outcome.
The lean design process inherently has a lot of inefficiencies as the team finds its rhythm together. Lean and inefficient are contradictions, often leaving designers shaking their heads and asking themselves, "What is the value in this process if there is inefficiency?"
The value is not clear at first, but the prize is what the project saves in construction and the operational efficiencies at occupancy. The key is to be patient and understand that while there is some necessary inefficiency in the process, it will pay off as the job progresses.
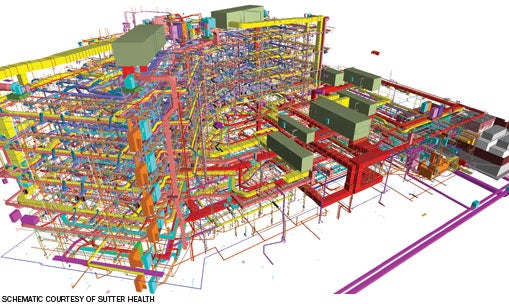 |
| A clash session will detect conflicts between the systems illustrated in this mechanical-electrical-plumbing schematic design model. |
Starting the process
As with any health care construction project, the technology design production flow starts with developing concepts through visioning sessions. These sessions chart how technology will facilitate the delivery of health care.
A key point in taking a lean approach is to understand and map how the data and communications must flow to match the flow of patients, staff and patient orders in the hospital. This is different from the way technology has been designed in the past.
Lean design moves away from just implementing systems based on tradition. Instead, the designer really must think about data mapping and communications, then add on the transport layer.
Technology designers usually are surprised at the result of this effort; many systems they thought were necessary in the past really aren't. They're finding other ways to accomplish the same technology mission. What should fall out of this mapping is a listing of potential data, communication and applications that can be implemented in the project.
The goal of the planning phase is to define the technology program and scope of work. In a traditional process, this would be a general description of the potential systems. In the lean process, the early stage of system definition must go further into detail to test the ability of the systems to bring leverage and help define the best strategy.
At the end of this stage, the following take-aways should be produced:
- A list of wired and wireless infrastructure that will support a broad array of technologies now and in the future;
- A listing and description of the systems and applications that are targeted for the facility as well as a listing of potential vendors for the systems;
- A preliminary space and equipment layout for main entrance facility and building distribution rooms as a test to fit;
- A preliminary layout for main-cable infrastructure pathways (e.g., cable trays, site raceways).
- A systems integration matrix defining how systems and applications might integrate with each other to share data and leverage each other for functions;
- A systems and applications matrix ranking risk of technology obsolescence and cost risk over the course of the project;
- A preliminary technology budget, with as much based on estimated quantity of items versus per square foot.
Modeling the design
The next step in the design production flow is tantamount to a preliminary design: actually laying out devices and infrastructure within a three-dimensional building model.
Compared with a traditional delivery model, this step occurs much sooner and looks a lot like what normally would be thought of as the schematics phase. The technology designer and all team members must realize that they are now in a dynamic process, stepping through it together as a coordinated team. There is less independent work and more collaboration as the designer forms the infrastructure and systems.
In the preliminary design phase, the technology designer is participating in several concurrent and collaborative tasks that include:
- Three-dimensional modeling of cable trays and pathways, and coordination of same with other building trades, primarily mechanical designers;
- Three-dimensional modeling and layout of all building distribution rooms for voice and data, including equipment rack and wall equipment layout;
- Preliminary specification of key systems that fall low on the matrix for technology change risk;
- Requests for proposal (RFPs) to select vendor partners for selected low-risk systems;
- Formal engagement of vendor trade partners as part of the team for selected systems;
- Systems cost-estimate updates, firming up numbers by using vendor quotes from RFPs.
Getting specific
The final part of the design production flow is where the detail design begins. Here is where shop-drawing documentation is happening — a step that, under the traditional design process, would not happen until construction.
With trade partners on board, it is now possible to coordinate fine-detail items from a spatial and connectivity point of view. The result of this effort is tighter-knit documentation.
But, perhaps even more importantly, trade partners have a vested interest in success so they work closer to minimize unwanted impacts of their design to other team members. Details that normally would be left to the field are worked out now because the team essentially is constructing the building in a three-dimensional virtual model.
Several key processes and outcomes are critical to the success of this part of the production flow, including:
- A fully coordinated, three-dimensional virtual building model with shop-drawing detail;
- Clash coordination between the trades complete with formal quality assurance and control accomplished;
- Buyout of most major technology systems and firm quotations for other systems;
- Pre-ordering of equipment that is low-risk for technology change if deemed necessary for scheduling purposes;
- Systems interfaces and middleware requirements defined and documented.
The right solution
Lean design for technology may or may not be the right solution for every project; however, new projects of a significant size certainly can be served well by the lean process.
Challenging the design team to innovate the traditional process bears positive results on the bottom line, both in construction as well as in operations.
Tom Leonidas Jr., P.E., is a health care practice leader and vice president at Sparling, a Seattle-based electrical and technology consulting firm that specializes in health care planning and design. He can be reached at tleonidas@sparling.com.
| Sidebar - 'Lean' process helps hospital upgrade systems at less cost |
| During the design and construction of Sutter Medical Center Castro Valley, a 231,000-square-foot replacement hospital in Castro Valley, Calif., the design team is finding that they have been able to streamline hospital processes and realize considerable cost savings. The hospital and regional trauma center, which is scheduled to open in January 2013, will offer an emergency department, surgery, birthing, diagnostic imaging, medical-surgical, universal care and an electronic intensive-care unit, among other departments. The design and construction team followed the lean production model with an integrated form of agreement (IFOA) under which the owner, design team and contractor are in a mutual contract that promotes collaboration. The technology design has been an iterative process, starting with an intense effort up front to map technologies to the clinical workflow. At the outset of this process, a long list of systems was created and budgeted for the project. The initial technology planning was based on a traditional systems approach that reflected the systems the hospital currently uses. This list of systems and attendant infrastructure was reflected in a cost budget. The challenge that the IFOA team gave the technology designers was to eliminate as many systems as possible without losing functionality. The other charge was to maximize integration between systems to share data and reduce operational maintenance. The third challenge was to integrate systems into the electronic medical record and with some select medical equipment, or at least provide the foundational building blocks to facilitate integration in the future. One of the key systems was a radio-frequency identification (RFID) asset tracking system that was able to use the 802.11 wireless network already designed into the building. The RFID system also was used to monitor temperature on medical refrigerators and freezers, which eliminated a separate monitoring system. There also was a request for a separate departmental intercom system that was fulfilled by using the Voice over Internet Protocol (VoIP) phone system handsets. Additionally, an IP-based security and video surveillance system was designed that could integrate easily with other systems. The process of defining details early on also opened doors to better integration strategies that were defined earlier for medical equipment and electronic medical records. This allowed the specifications for the medical equipment as well as the electronic medical record deployment to have better definition, providing a better sense of cost and implications. By going through the lean production process, the technology design was able to eliminate five systems that originally were thought to be needed, bringing about a 10 percent savings for the technology budget. The savings was available to fund other wish-list systems. |