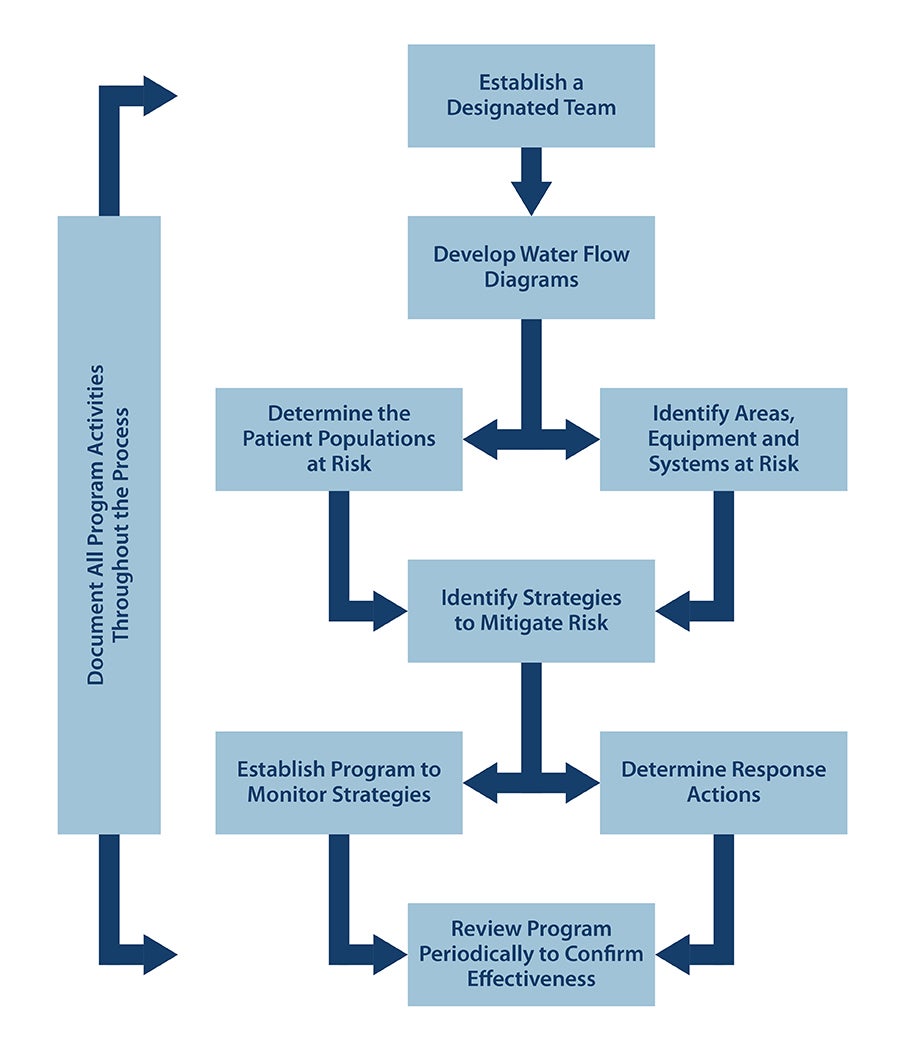
Activating a water management plan

An important aspect of implementation is a functioning team that can effectively oversee the water management program.
Images by Getty Images
Implementing an effective water management program prepares hospitals to meet challenges associated with waterborne pathogens and water system hazards in general.
The American Society for Health Care Engineering’s recently released monograph, “Water Management in Health Care Facilities, Second Edition,” outlines how to put together an effective water management program.
This article is excerpted and edited from that 60-page monograph.
Create the team
Perhaps the most important aspect of implementation is creating a functioning team that can effectively oversee the program, referred to as the “designated team” in some standards.
Facilities should establish the team and then have it oversee writing the water management plan. This team could be a component of the environment of care committee or the utility management team within the hospital.
An effective team should have clear objectives, balanced roles, effective communications, defined responsibilities and appropriate leadership. Depending on the organizational structure, it should have a defining charter and/or management protocol providing clear direction.
The team’s purpose is to write an implementable water management program and operating procedures that effectively reduce the risk of waterborne pathogens and oversee effective implementation of the plan. Team member roles should include:
Hospital executive. The hospital executive should be able to provide sufficient resources to the team and report significant issues, findings and risks to senior leadership. They also must have the authority to make command decisions about the program.
Facilities manager. Someone very familiar with building water systems must be on the team. They should have the ability and authority to provide maintenance resources, report findings and make command decisions as they pertain to the program.
Infection preventionist. Someone familiar with the health care facility’s infection prevention protocol and methods of reducing the possibilities of infections must be on the team. This person should be an accredited and degreed epidemiologist or otherwise certified in infection control. They should be familiar with the areas occupied by at-risk patients, able to provide recommendations regarding the findings from facilities management and assist with water management decisions.
Additional team members should be considered from the following areas:
Nursing management. This person should be able to provide resources to support appropriate actions for water management program implementation.
Occupational and environmental safety management. This person should provide appropriate resources to assist with understanding the findings and supporting the decisions of the team.
Representatives of affected areas. These people should have the authority to implement the water management actions within their designated areas.
Others. Other experts, either inside or outside the facility, can be included.
The team should meet at regular intervals to ensure proper implementation and maintenance of the plan. When the plan is first implemented, the team may need to meet more frequently. It also should meet more frequently when significant issues are discovered and intervene immediately when epidemiologically indicated.
If writing the detailed specifics of the water management plan is beyond the skill set of the team, it may seek the support of an engineer with waterborne pathogen experience, an infection preventionist, a water treatment specialist or an industrial hygienist.
Map the system
The team should obtain or develop a water system flow diagram of the entire building water system to help identify potential hazard conditions and high-risk patient care locations.
The diagram should include all water supply sources, treatment systems and control measures, processing steps and end-use points. It also should include all areas occupied by at-risk patients. Lastly, the flow diagram should identify equipment where water may be aerosolized, including cooling towers, pools, spas and whirlpools, non-steam humidifiers and ice machines.
Everyone on the team must understand how water flows through the building — where it enters and how it is filtered, pumped and distributed. Not everyone on the team needs to be a subject matter expert, but all should understand the systems. Consideration should be given to having the designated team tour the facility to establish a base-level understanding.
The hospital should keep easily accessible diagrams illustrating the current state of the water distribution system. This is necessary during any critical water situation. It also is helpful when planning construction and can generally help reduce water system-associated risks. Accrediting organizations also require that utility systems be properly designed, installed and mapped.
Current plumbing as-built drawings could be used as the water system flow diagram but may be too complicated to be used to assess risks. A simplified diagram may be more useful. The flow diagram should include all the areas and equipment where hazardous conditions may exist as well as locations occupied by high-risk patients.
Design the plan
The designated team should use the water system flow diagram to help create the water management plan. All aspects of the water management plan must be documented, including development, implementation, verification and validation. In addition to the water system flow diagram, the plan should include:
Contact information. The plan should include the name, title, role on team and contact information for all team members.
Systematic evaluation. The team should evaluate the physical and chemical conditions of each step in the water system flow diagram to identify where hazardous conditions may occur. Then, it should identify areas where patients have a reduced immunity level and higher probability of infection. Using these two factors, the team should estimate the likelihood of waterborne pathogen risk in locations throughout the water system.
Waterborne pathogen risk assessment. While taking the systematic evaluation into account, the waterborne pathogen risk assessment should follow the facility’s infection prevention and risk management protocols. Considerations for assessing risk include:
- Determining whether the facility has experienced a case of facility-associated or indeterminately caused waterborne infectious disease in the past.
- Considering whether the supply of water to the site poses a high risk for waterborne pathogens. The facility should test and document disinfectant levels from the municipality and temperature from the incoming source at the change of seasons for surface water or annually for well water.
- Over time, the documentation provides data that could establish baseline information for a dashboard indicator of normal operations. Variations should be brought to the team for discussion and risk analysis.
Control locations and limits. The systematic evaluation is used to identify areas of higher waterborne pathogen risk where a control measure may be desirable.
American National Standards Institute (ANSI)/ASHRAE Standard 188, Legionellosis: Risk Management for Building Water Systems, and ANSI/ASHRAE Standard 514, Risk Management for Building Water Systems: Physical, Chemical, and Microbial Hazards, require that the water management plan outline the procedures required for prevention and control of waterborne pathogens.
The systematic evaluation is used to identify control locations and establish control limits, which are a range of acceptable values associated with a chemical or physical parameter for identified control locations. These control limits could refer to characteristics such as water flow rate, water temperature, disinfectant residual, concentration of pathogen or another identified parameter.
At these control locations, the designated team may implement a control measure to help ensure the location stays within control limits. Possible control measures include disinfecting, heating, cooling, filtering, flushing or other means, methods and procedures to maintain the water within the control limits.
Monitoring control measures. Water management standards require the development of procedures to monitor control measures. This is a planned sequence of observations or measurements of the physical and chemical characteristics of control measures.
By monitoring the incoming water and systems within the facility, the team can identify deviations from normal operations and whether the deviation is a fluctuation in the system, which can be indicative of a potential change in risk for waterborne pathogen detection.
If values are outside of control limits, the water management plan needs to identify corrective action to bring water characteristics back within the established control limits.
ANSI/ASHRAE standards 188 and 514 are not prescriptive. The framework relies on the team to construct a system that reduces risk within a facility.
Maintenance protocols. The team should ensure that standardized maintenance protocols are adequate and followed. In addition, maintenance protocol development should be based on best practices for each piece of equipment. Standard maintenance should be performed at the correct intervals by knowledgeable facilities maintenance staff or outside vendors. All work must be documented.
The team should develop procedures that address the areas required for a utility management program, such as shutting off malfunctioning systems, obtaining emergency repair services and responding to disruptions to water systems.
Whenever there is an elevated risk, the water management plan must indicate procedures to follow. These might include notifying infection prevention, facilities management and provider staff of the risk.
The water management plan should indicate procedures to follow when infection control identifies a probable or waterborne pathogen case. It also may indicate under which circumstances testing for Legionella and other waterborne pathogens might be performed.
The team should develop contingency response plans that detail procedures if there are known or suspected cases of diseases associated with waterborne pathogens. These plans should include criteria indicating when and where testing should be performed, procedures for emergency disinfection or other remedial actions, procedures for emergency clinical interventions and recommendations from health department authorities.
Procedures should include following established infection control processes and applicable laws, implementing remediation actions and reevaluating the water management plan.
Periodic review. The team also should develop procedures to confirm that the water management plan is implemented as designed and effectively controls hazardous water conditions within the building water systems. This confirmation could be as simple as generating a reporting spreadsheet for specific steps within the water management plan and reviewing with the designated team when there are anomalies. It should include a review of the maintenance documentation.
Develop the procedures
Robust building water system procedures are an effective way to reduce the risk of waterborne pathogens. ANSI/ASHRAE standards 188 and 514, as well as the ANSI/Association for the Advancement of Medical Instrumentation ST108, Water for the processing of medical devices, require the water management plan to include design and installation of utility systems as well as system evaluation and building surveys. A closer look at these elements includes:
Design and installation. Health care facilities should proactively evaluate and select equipment with the best possible low-risk design to ensure safe system operation.
Design of the water distribution system should include means and methods of disinfection before occupancy and during outbreak conditions. Extra investment to ensure the system minimizes any risk of biofilm or pathogen growth should be considered. Additionally, the team should have final authority to accept or reject any value-engineering recommendations.
System evaluation. The team should evaluate the building water management plan on an annual basis. At minimum, the evaluation should include:
- A review or update of the building water flow diagram to determine if any changes add new hazard points and if any new equipment or systems may generate aerosols.
- A review of the areas occupied by at-risk patients to determine if changes in clinical practices increase or decrease at-risk patient areas and whether any additional water-using equipment has been installed.
- A review of monitoring activities to assess the results of the risk mitigation strategy monitoring and make any changes in control ranges or maintenance intervals.
The results of this evaluation should be reviewed and summarized to organization leadership. One way to accomplish this may be to include the summary report in the utilities management program periodic reports through environment of care reporting and as a portion of the annual evaluation report of the utility management program.
Plan of action
Health care leaders should have a general sense of what is necessary to protect patients, staff and visitors from hazards associated with building water systems.
Without proper guidance, facilities may take steps that are not required, are unnecessarily costly or are not helpful in reducing the threat from waterborne pathogens.
A good water management program gives a facility the best plan of action to mitigate as much risk as possible.
This article was excerpted and edited by Health Facilities Management staff from the American Society for Health Care Engineering’s “Water Management in Health Care Facilities, Second Edition” monograph.
Related article // Exploring the three standards
The three different water management standards addressed in the American Society for Health Care Engineering’s (ASHE’s) “Water Management in Health Care Facilities, Second Edition” monograph each have the primary focus of protecting users from waterborne hazards. However, each has been developed to address different aspects of water quality and safety, with its own scope and purpose.
For instance, the American National Standards Institute (ANSI)/ASHRAE Standard 188, Legionellosis: Risk Management for Building Water Systems, focuses on Legionella control, while ANSI/ASHRAE Standard 514, Risk Management for Building Water Systems: Physical, Chemical, and Microbial Hazards, expands to encompass a broader range of microbial, chemical and physical hazards in building water. Additionally, ANSI/Association for the Advancement of Medical Instrumentation ST108, Water for the processing of medical devices, is tailored for water used in sterilizing and cleaning medical devices.
Appendix D of the ASHE monograph provides a comparison matrix of the three standards and an overview of several different categories. Regarding health care specificity, the monograph states:
- ANSI/ASHRAE Standard 188. Annex A of Standard 188 addresses health care needs, requiring infection prevention protocols and system mapping specifically for hospitals and health care facilities.
- AAMI ST108. This is highly specific to health care facilities, addressing water quality concerns critical to the safety of device processing and patient outcomes.
- ANSI/ASHRAE Standard 514. This standard includes health care-specific guidance with special requirements for health care buildings, supporting infection control, patient safety and facility-specific risks.
The comparison matrix was developed by the monograph authors to help provide a quick overview of the three standards, how they differ and how they work together to provide a more in-depth and comprehensive water management program.
Because there are many different dangers, health care organizations should develop a comprehensive water management program that encompasses the appropriate aspects of water management standards based on the organization’s patient population, services provided and potential risks.
The matrix in Appendix D provides key information on how to align important aspects of a water management program.
Sidebar by Jonathan Flannery, MHSA, CHFM, FASHE, FACHE, senior associate director of ASHE Regulatory Affairs.