Designing for emergencies
 Increased growth in volume, pressures for operational efficiency, new operational models for patient flow and new concepts in physical design make planning for emergency services space a complex problem with at least four basic questions:
Increased growth in volume, pressures for operational efficiency, new operational models for patient flow and new concepts in physical design make planning for emergency services space a complex problem with at least four basic questions:
- How do you estimate space needs?
- What new operational concepts are emerging in emergency operations and what are their implications for design?
- What are the major design topologies for emergency services?
- How can you assure safety under typical operations and how can you design for surges resulting from natural and man-made adverse events?
A successful plan for designing emergency services space would examine each of these questions to develop solutions that apply to a given facility.
Estimating space needs
A basic question in emergency planning is the trade-off between assuring quick patient access to treatment and the operational and facilities cost requirements to meet peak-demand periods. One dimension of this problem is quantifiable — estimating peak demand and resulting bed needs. Determining the acceptable level of delays is a function of the patient mix as well as the institution's values, strategic vision and resources.
A useful model for the analysis of such complex services as emergency care is Eliyahu Goldratt's "Theory of Constraints," which is discussed in his 1990 book of the same name. This approach seeks to identify components of a system that inhibit the flow of events.
In the case of emergency departments (EDs), designers look for factors that affect the processing and movement of patients. From a facility perspective, they should seek to identify the physical resources, particularly treatment spaces. If successful, designers will identify the minimum building resources to assure that space is not the constraining variable.
To achieve this goal, designers need to understand the demand during peak periods and then determine the required resources. The problem typically is divided into two components:
- Analysis of the external variables that create demand that are not in control of the ED; and
- Assessment of the internal operational processes and resources that are available to respond to the demand.
External components that should be included in the projection of demand include population demographics, utilization patterns, market share characteristics, anticipated health care policies and the strategic vision of the institution.
Analysis of historical use patterns provides one important starting point in identifying peak-periods demand. Four components of patient-visit patterns typically are included in this analysis. Three usually are consistent and stable for individual institutions. However, the fourth variable — total volume projections — has been the downfall of many studies.
The three components of demand that are reasonably consistent and can be analyzed with departmental historical data are peak month of the year, peak day of the week and peak arrivals by hour. The combination of these factors can be studied to translate total projected visits into peak-period arrival patterns. Ideally this will include the inter-arrival patterns (average minutes between arrival) during peak periods for patients by such major categories as major trauma, pediatrics, behavioral and urgent care.
Over the past 20 years, the total annual visits has proved the hardest to estimate, with projections frequently underestimating the true demand. Factors that have contributed to these underestimates include the overall population growth and the aging of the population, the increasing utilization rates (visits/100) in major age cohort categories and the closing of hospitals and trauma centers across the country. Nationally, visits to EDs have increased at an average annual rate of 2 percent. Many new EDs have reported an additional 5 percent to 10 percent initial jump in visits at the opening of a new facility.
One planning tool that can be useful in addressing potential demand is scenario analysis. This seeks to combine a wide range of factors affecting future demand into groupings of two or three alternative futures. Analysis of space needs can be tested against these alternative futures to understand the potential range of space needs. Common physical needs and unique requirements of each scenario can be used to decide on a preferred plan.
Patient flow models
The organization and physical shape of many emergency services have gone through dramatic changes as hospitals seek solutions to overcrowding, increasing lengths of stay, and risk associated with man-made and natural disasters. Pressure to accept existing patient processes and lengths of stay must be resisted to assure that future plans do no more than institutionalize existing problems. Careful examination of the patient process and options for improving the patient experience must be undertaken parallel to the external analysis to assure that the pieces are in place to design a functional health care facility.
Applications of lean analysis techniques to emergency services by Jody Crane, M.D., Christopher De Luca, M.D., Kevin Roche and others have resulted in innovative methods for managing the front end of the patient process and the use of facilities to support efficient staff utilization.
One concept in these new approaches is to radically reconfigure the triage function and the management of low and moderate acuity patients. Emergency services are developing "chair-centric" concepts that move patients quickly into spaces in which a treatment team, including nurse and provider, can assess patient conditions, provide minor treatments and manage disposition for selected patients.
Results waiting and internal waiting areas also are being used to assure that treatment spaces can be turned during peak periods to maintain patient flow. Reductions in length of stay in the treatment areas can be dramatic, increasing the throughput of each area and reducing the total space required for the department.
Once a working model of the desired patient flow is defined and target lengths of stay in treatment areas are established, simulation models and other tools can be used to estimate the required number of treatment stations. This will serve as one of the bases for the functional space program and project budget.
Over recent projects, the ratio of departmental gross square feet (DGSF) to treatment area has fallen in the range of 650 to 750 square feet. Most institutions are moving to all-private-room models.
Design topologies
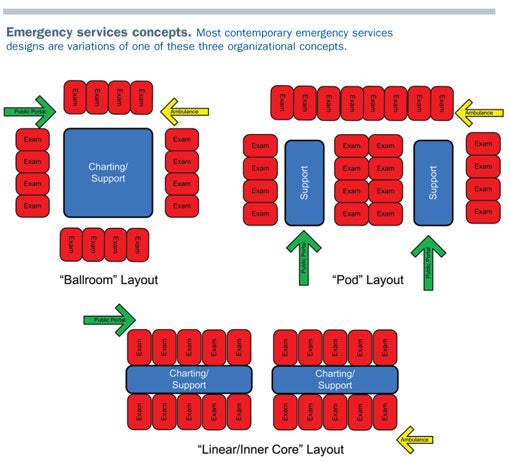
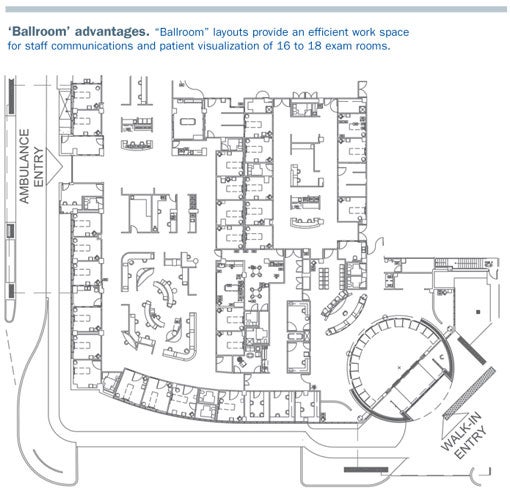
Contemporary design concepts can be grouped into variations of "ballrooms," "pods" or "inner-core (linear)" configurations. Thirty years ago, the predominant model was the ballroom layout, which wraps patient care stations around a central working area. This allows maximum visibility of patients and easy control of the departments.
As workload volumes increased and as more departments moved to private patient rooms, the functional limit of the ballrooms was reached at 16 to 18 rooms. A larger unit does not allow staff to observe all patient care areas and the size of the staff work area starts to become disproportionately large.
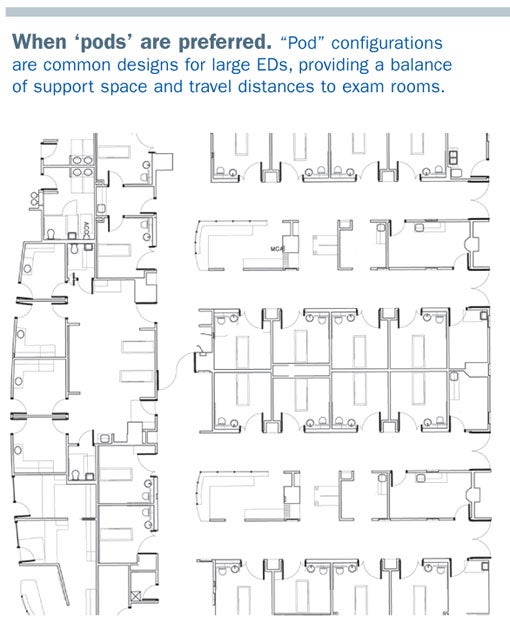
One alternative to this layout is the pod design, which groups clusters of 8 to 12 exam rooms together with a support area and internal circulation to other pods. This provides the opportunity to maintain efficient staff travel and balance between support space and treatment areas. A potential limitation of the design could be an inability to staff pods efficiently during periods when patient workloads are rapidly increasing or decreasing.
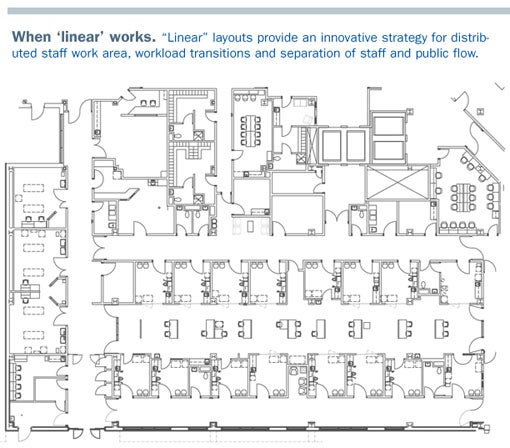
A third organizational concept is emerging as a design solution to increase volume, provide expansion potential and aid staff efficiency.
This inner-core concept, pioneered by Jim Lennon, AIA, ACHA, organizes treatment rooms around a staff work area. Rooms are dual entry, with patients and family accessing the treatment rooms from a perimeter corridor. Conceptually, staff work in decentralized zones supporting 10 to 12 exam rooms. These zones are staffed up and down to match the typical increase or decrease in patient volume throughout the day. If positioned correctly, expansion of the ED could be achieved logically and efficiently.
Adverse-event planning
Providing emergency services during disasters and epidemics has become important during the past decade. In addition to planning for normal operations, assessment of potential adverse events that could create demand or unique needs should be part of the design process.
Significant research into design considerations was undertaken in the ER One study (www.whcenter.org/body.cfm?id=555603), sponsored by the Office of Homeland Security. This study was directed by Mark S. Smith, M.D., Washington Hospital Center, and a team of physicians, architects and planners.
One of the first designs using ER One concepts is Tampa (Fla.) General Hospital. A full-day workshop was organized during the programming and early design process to address emergency preparedness. Hospital administration, ED staff, other employees, and security and community agencies completed a risk-assessment analysis to identify potential risks (e.g., hurricane, pandemic epidemic or direct attack on the ED), the probability of occurrence (e.g., high or low) and the potential facility implications. Events with a high probability and significant facility implications were studied in more detail, with specific recommendations developed for the planning.
Discussions with the State of Florida, the project architects (Gresham, Smith and Partners) and hospital administration led to a concept that allows the ED to expand from 77 treatment locations to 210 within the department space. A parking area beneath the ED also can convert from valet patient parking to a mass decontamination zone, feeding directly into the ED. Additionally, the patient holding and observation area is designed to convert to a quarantine unit, with direct access from outside the department for patients and families during potential high-risk epidemics.
By identifying these requirements during planning, the net capital cost impact on the overall project was held to less than five percent of construction.
The appropriate design
Evaluating which design is appropriate should be based on performance criteria established in consultation with administration and the ED staff. Suggested criteria answer the following questions:
- Does the design provide efficient patient flow?
- Are work areas, supplies and medications located to minimize staff travel?
- Are work areas designed to maximize staff interaction and visual connectivity?
- Can the ED staff up and down during the day to respond to patient demand without creating unnecessary queues or inefficient staff ratios?
- Can the ED functionally respond to high-risk potential events?
- Is the design flexible to accommodate future growth through internal adaptation or expansion?
- Is the design efficient from a square-foot-per-treatment perspective?
The design team should seek to achieve the goal frequently proposed by the health care futurist Leland Kaiser: "The future is too important to guess at, you need to invent it."
Frank Zilm, D.Arch., FAIA, FACHA, is president of Frank Zilm & Associates Inc., Kansas City, Mo. He is the Chester Dean lecturer on health care design at the University of Kansas and has served as president of the American Institute of Architects Academy of Architecture for Health. He can be reached at frank@zilm.com.
| Sidebar - Resources on designing for emergency services |
| Need more information on designing for optimal emergency services? Check out the following resources, which the author used to prepare this article. Books Theory of Constraints, Eliyahu Goldratt, North River Press, Great Barrington, Mass, 1990 Journal articles Optimizing Emergency Department Throughput: Operations Management Solutions for Health Care Decision Makers, John Shiver and David Eitel, Productivity Press, New York, 2009 |




