FGI provides updated guidance on designing mobile medical units

Rendering shows layout of a mobile magnetic-resonance imaging unit featuring scanner technology in a dedicated trailer.
Image courtesy of Siemens Healthineers
Mobile/transportable medical units have been used for many years throughout the United States to provide temporary access to medical and dental services, diagnostic imaging and other nonemergency services.
However, in recent years there has been an increase in the acuity level of patients being served in these units, and the medical services provided have become more complicated and more invasive. In fact, these services are often the same as those offered in permanent structures, but are being provided in spaces without the same oversight and regulation.
Because a mobile unit is not defined as a building, it is not regulated by building or fire codes. Additionally, most of the facility-design requirements developed by the Facility Guidelines Institute (FGI) for hospitals and outpatient facilities are directed at a building environment rather than a mobile unit. Although previous editions of FGI’s Guidelines for Design and Construction provided some design requirements for mobile units, these standards were not sufficient to ensure patient safety for the various services and procedures currently offered in this setting.
The following overview of some of the major revisions to the chapter, retitled “Specific Requirements for Mobile/Transportable Medical Units,” which appears in the 2018 editions of the FGI Guidelines for Design and Construction of Hospitals and the FGI Guidelines for Design and Construction of Outpatient Facilities, provides those in health facility operations and design with a glimpse at where this growing venue is heading.
Preliminary issues
During the 2018 Guidelines revision cycle, a task group was formed to review the 2014 Guidelines chapter on mobile, transportable and relocatable units. It was charged with revising the chapter to meet the goals of supporting patient and staff safety for all medical services provided in these units and to assign responsibility to ensure that these conditions are met.
The first issue the task group had to resolve was assigning responsibility for the initial design and construction of a mobile/transportable unit and for its ongoing maintenance. Unlike a building, a mobile/transportable unit often is relocated to different service sites that are operated by different owners and regulated by different authorities having jurisdiction (AHJs).
The task group decided to treat the mobile unit similarly to a piece of medical equipment brought into a health care facility and to provide several ways these units could be “certified” for initial installation. Permitted methods of certification include signing and sealing of the manufacturer’s construction documents by the design professional who initially designed the unit; using a third-party, nationally recognized testing laboratory (NRTL) certification or labeling of the unit; or another certifying means acceptable to the AHJ, such as professional association certifications.
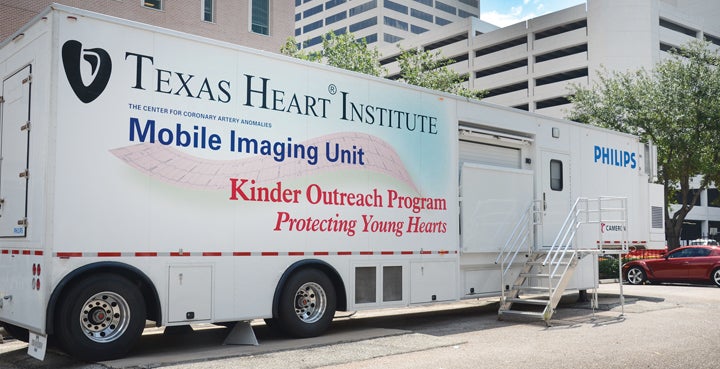
Texas Heart Institute in Houston uses its mobile imaging unit to help move care into the community.
Image Courtesy of Texas Heart Institute
At this time there are no NRTLs that certify mobile medical units, nor is there a professional association that has written any standards for them. Thus, at present, the vendor of the unit is responsible for ensuring that it has been designed and constructed to the Guidelines standards. After initial installation, the host facility or the medical-unit owner or lessee is responsible for keeping records of all maintenance, as is required for any piece of medical equipment in a patient care area. Each time the mobile/transportable unit is relocated to another facility for service, all systems must be retested and a written record maintained by the host facility, indicating continued compliance with applicable codes and standards.
The next issue the task group identified was the connection between services provided and design standards required. It was determined that patient-safety design standards should be based on the types of medical services to be provided in a unit rather than the setting in which those services take place. Just because services are provided in a mobile unit does not mean that the minimum design standards for patient safety can be ignored. The task group wanted to find a way to scale reasonable requirements based on the types of services provided.
Concurrent with the work of the mobile units task group, an imaging task group developed a classification system of room types for imaging services based on the procedures performed in those rooms and the risks to the patient. This work was reviewed and adapted to designate classes of mobile/transportable medical units based on increasing levels of medical intervention.
Three categories of services were identified with a varying degree of adaptability for each class:
- Class 1 medical units are used for such services as diagnostic radiography, fluoroscopy, mammography, computed tomography scan, ultrasound, magnetic-resonance imaging (MRI) and other completely noninvasive imaging modalities.
- Class 2 units are those in which procedures are performed such as diagnostic and therapeutic coronary, neurological or peripheral angiography procedures and endoscopic procedures.
- Class 3 units are those in which invasive procedures are performed requiring physiological monitoring and active life support for the patient.
As part of their review of the mobile units chapter, the task group decided to omit the “relocatable/modular” unit types because these units are not designed to be mobile once they’ve been placed in service and therefore are no different from a building structure.
General design requirements
Once the broader, preliminary issues were resolved, the task group developed general design requirements that apply to all three unit classes.
Access to the site must be provided for a unit, including the necessary turning radius and a safe location for the unit on level ground at least 25 feet from any air intake in the host facility. If the unit is situated close to a driveway, it must be protected from accidental impact. A unit in which MRI is provided must be located so that persons near the unit are not harmed by the magnetic field.

The Siemens mobile magnetic-resonance imaging solution provides the same diagnostic performance as fixed scanners located in a hospital.
Image courtesy of Siemens Healthineers
Protection from the weather is needed for patients entering the mobile unit from the host facility. If an outdoor covered walkway is used, it must meet all building and fire codes. If the walkway is constructed as interior space, it must be separated from the host facility by a two-hour, fire-rated separation wall. In both cases, this connector cannot interrupt the required egress from the host facility or the unit.
Site utilities, including electrical, mechanical and plumbing systems, must be either available to the unit from the host facility or self-contained inside the unit. Utility design requirements for the unit itself, such as HVAC, electrical and nurse-call standards, are provided in the “Common Elements” chapter of the 2018 Hospital and Outpatient Guidelines documents.
For example, Class 1 units must meet the requirements of ASHRAE 170, Ventilation of Health Care Facilities, for outpatient facilities that require positive- or negative-ventilated areas, while all areas of Class 2 units must meet all ASHRAE 170 ventilation and filtration requirements for the identified areas.
A fire-alarm system with a pull station must be located inside the mobile unit with a connection to a 24/7 staffed location of the host facility.
Waste must discharge into the host facility’s sewage or into a storage tank in the unit. Freeze protection must be provided when required by the geographic location. If piped medical gas is used, it must conform to the requirements of the National Fire Protection Association’s NFPA 99, Health Care Facilities Code.
- New Class 1 and 2 unit design requirements: For Class 1 and 2 units, the task group identified a few alternative methods for compliance with the Guidelines sections that relate to the services offered when they are provided in a building. These alternative methods include the following:
- Where room dimension requirements in the Guidelines cannot be met, dimensions sized to accommodate equipment and personnel must be incorporated in a complete risk assessment provided to the AHJ for approval.
- For Class 1 units, holding areas may be located in the unit or “readily accessible” to the unit (defined in the Guidelines glossary as “on the same floor”), so may be in the host facility if on the same level as the mobile unit. Class 2 recovery areas may be located in the unit or “adjacent” to it, which is defined as “located next to but not necessarily connected to the identified area or room,” again allowing placement nearby in the host facility.
- Some supporting spaces required when health care services are provided in a building (e.g., patient changing areas, patient toilet rooms, clean and soiled utility rooms, storage rooms and holding areas) are permitted to be located in the host facility if they are readily accessible to the mobile unit.
- New Class 3 unit design requirements: Class 3 units must meet all of the standards for the services performed as described in the Guidelines for a permanent building. Class 3 mobile units are defined as those in which clinical services require physiological monitoring and active life support for the patient receiving treatment, which means that they are basically mobile operating rooms. Thus, the task group agreed that no variations from the minimum requirements for patient safety could be permitted when these invasive procedures take place inside a mobile unit. The minimum clear floor area and clearances; accommodations for equipment; and all architectural, mechanical, and electrical minimum requirements detailed in the Guidelines facility chapters must be met inside a Class 3 mobile unit.
Maintaining safe facilities
Previous Guidelines editions did not provide sufficient specific details to ensure patient safety for diagnostic and treatment procedures provided in a mobile/transportable unit.
By employing a tiered arrangement based on the degree of interventional services provided, the revised 2018 design requirements support a physical environment that is safe for patients, allowing mobile/transportable units to remain an important means of extending temporary medical services into the communities they serve.
Skip Gregory, NCARB, a health care code consultant based in Tallahassee, Fla., chaired the mobile/transportable medical units task group for the 2018 Health Guidelines Revision Committee. He can be reached at gregoryskip@gmail.com.